Search Posts
Recent Posts
- Washington Bridge moving to 6 tight lanes – time for good situational awareness April 19, 2024
- Rhode Island Weather for April 19, 2024 – John Donnelly April 19, 2024
- Homeless in RI: Opening of Providence pallet shelter community delayed – Rhode Island Current April 19, 2024
- Outdoors in RI: Rainy days and fishing, We the People, customer service, 2A update – Jeff Gross April 19, 2024
- GriefSPEAK: Voir Dire – Mari Nardolillo Dias April 19, 2024
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.

The 15-minute office visit has been forever changed – Richard Asinof
by Richard Asinof, ConvergenceRI
This article is by Gail Patry and Dr. Rebekah Gardner, MD
[Editor’s Note: As the COVID pandemic keeps shifting shapes, so, too, do the responses by the health care delivery system. The 15-minute office visit, once the staple of how patients experienced the delivery of health care, has forever been changed into a hybrid vehicle – a mixture of telehealth visits, remote monitoring check-ins, and minimally invasive, in-person interactions.
As detailed in the 2020 ConvergenceRI story, “From a novelty to a necessity,” new innovations and new technologies were deployed by Healthcentric Advisors, in order to meet “the need to ‘see’ patients and ‘talk’ with them, monitoring their conditions, without putting the providers or patients at further risk for possible contamination from the virus.” [See link below to ConvergenceRI story.]
Three years later, Healthcentric Advisors has published the research of what it found were the results of the deployment of this innovative technology. Here a story reporting on what those findings were – and what they promise for future changes in health service delivery.]
The pandemic spurred many changes in health care delivery, including significant advances in telemedicine and remote monitoring services for chronic conditions, such as hypertension, diabetes, and chronic obstructive pulmonary disease [COPD].
Healthcentric Advisors, a nationally recognized quality improvement consulting organization, began expanding its remote monitoring services to meet this increased need for practices in New England, in order to ensure individuals would continue to receive the care for these conditions that they need, despite having less in-person access to their primary care physicians.
Remote patient monitoring [RPM] leverages technology to obtain patient data virtually, in addition to information obtained during an office visit. It offers significant benefits to the overall care of individual patients as well as the health care delivery team.
A recent research study conducted by Florence Kariuki, RN, in 2022, found several significant benefits to using technology for remote patient monitoring.
They included:
• Improvements in proactive care delivery in between visits
• Increased patient engagement in self-management and decreased cost [for in-person visits] as well as increased access to care, resulting in increased patient satisfaction
• Reduced health care expenditures on avoidable Emergency Department usage and hospitalizations
• Increased practice revenue in addition to increased staff efficiency [critical in light of today’s clinical staff shortages]
Necessity is the mother of better health care delivery
What started as a remote blood pressure monitoring pilot program under a contract with the Centers for Medicare and Medicaid Services [CMS] expanded to include blood sugar/Hemoglobin A1C, weight for congestive heart failure [CHF], and pulse oximeter readings for chronic obstructive pulmonary disease [COPD].
Key pilot results, including rates of improvement in blood pressure readings and level of patient engagement, were proven to be important drivers in expanding the program.
The average in-person patient appointment with a primary care provider is 15 minutes. Translated, the goal of this program is to maximize what happens in the other 1,425 minutes in a patient’s day.
The patient was able to stay connected to their care team easily through conveniences such as: working on smart phones, flip phones, tablets, and computers; using only internet not Wi-Fi; being translated into Spanish and Portuguese; and allowing patients to request a call from the care team.
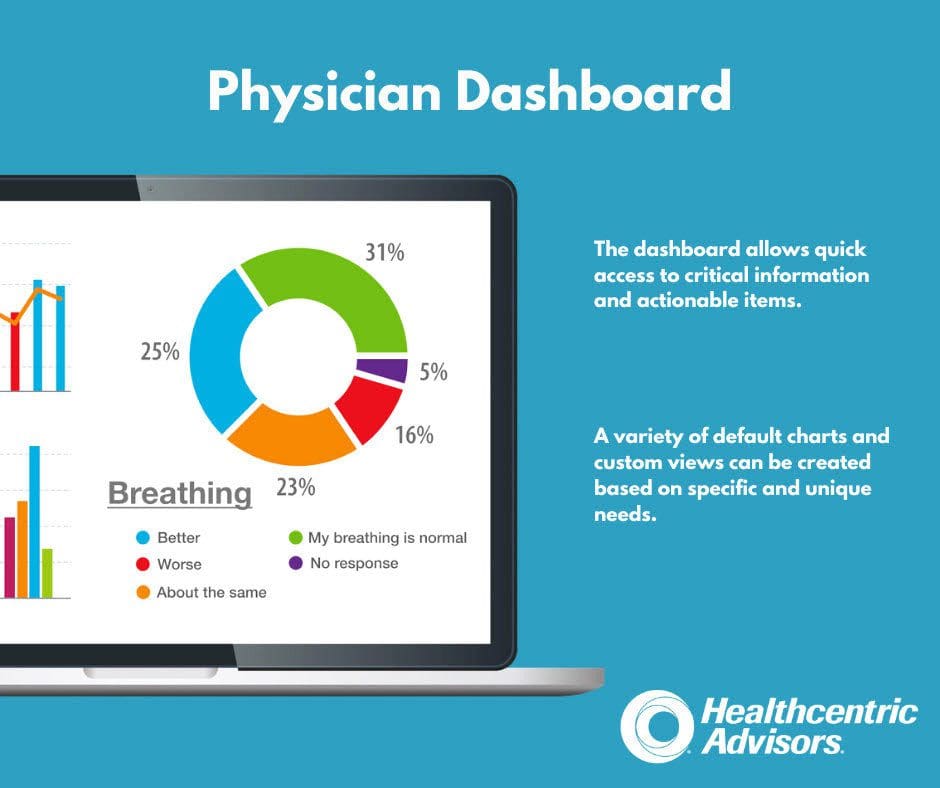
According to a study conducted by Dr. Rebekah Gardner [2022], the Healthcentric Advisors portal, known as PRiSM, resulted in real-time patient outcomes, as well as significant efficiencies for the practices caring for them.
• Among the 5,532 patients who used PRiSM for COVID symptom monitoring, 78 percent of the daily texts resulted in a response from patients.
• Most patients agreed that responding to texts was easy [95 percent] and that they would be willing to participate in other texting programs [78 percent].
• Most staff agreed that the program reduced burden of outreach [94 percent] and that they would recommend use to other practices [100 percent].
• Among patients using PRiSM to monitor blood pressure, 79 percent reported an increased ability to manage their blood pressure.
Positive vibrations
Patients and their care teams offered positive feedback on the remote monitoring programs. Here are a few specific quotes and examples:
• “Using [the PRiSM] INSIGHTS dashboard, I realized a patient gained weight via her weight entry in the portal on a Friday afternoon. With PRiSM, I was able to call her to verify her weight entry was correct, [then] conferenced… our Nurse Care Manager to join in on the phone call. The diuretic was sent to the pharmacy before the weekend. What historically would have likely resulted in a weekend admission was avoided by this key information before the weekend, allowing for care-team intervention.’
• “I feel better knowing they are there monitoring me, supporting me, and ready to help.”
• “This is no doubt a program that will save lives or in my case, add years to my life.”
• “Happy to be in the program. My BP is under control. And I’ve never felt better.”
Financial implications
Of course, no conversation about health care is complete without talking about the financial implications.
The good news is RPM is reimbursable through Medicare [following specific reimbursement guidelines], and practices have reported that it allows them to maximize the staffing resources they have available to them to provide care management services to their patients.
Another significant financial benefit is in cost avoidance – for patients, and for insurance plans such as Medicare, as patients who have participated in the program have experienced significant less need to access emergency department services or hospitalizations.
Gail Patry, MS, RN, is the Senior Vice President of Quality Programming at Healthcentric Advisors. Dr. Rebekah Gardner, MD, is the Senior Medical Scientist at Healthcentric Advisors.
[For more information, contact the PRiSM staff at Healthcentric Advisors, Melissa Miranda, at [email protected], or [email protected]].

[Editor’s Note: Healthcentric Advisors is an award winning, nonprofit, health care quality improvement and patient safety advisory organization, headquartered in Providence. They partner with federal and local government agencies, foundations, insurers, health care providers, human services agencies, educational institutions, and other private and community organizations to improve the quality of health care being delivered and the overall health of the communities served.
Their areas of expertise include: quality improvement and patient safety; health care performance and outcomes public reporting; research, analytics, and program evaluation; safe transitions, care coordination, and readmissions reduction; physician and ambulatory care health information technology [HIT] optimization; practice transformation and value-based care support; and specialized project management, implementation, and research.]
___
