Search Posts
Recent Posts
- Washington Bridge moving to 6 tight lanes – time for good situational awareness April 19, 2024
- Rhode Island Weather for April 19, 2024 – John Donnelly April 19, 2024
- Homeless in RI: Opening of Providence pallet shelter community delayed – Rhode Island Current April 19, 2024
- Outdoors in RI: Rainy days and fishing, We the People, customer service, 2A update – Jeff Gross April 19, 2024
- GriefSPEAK: Voir Dire – Mari Nardolillo Dias April 19, 2024
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.

COVID symptoms different in older patients – Richard Asinof
New research points to the need for better, improved testing
There remains so much to learn, from a medical research standpoint, about the coronavirus pandemic, and the different ways that it afflicts the human body – and the need to develop treatments that reflect the new scientific research as it becomes available.
One of the researchers at the forefront, it turns out, has been Dr. Elizabeth Goldberg, MD, who, with her colleagues, recently published a study that, as Goldberg described it, “sheds light on age-related differences in symptoms of COVID and health outcomes.
“
Here is the ConvergenceRI interview with Dr. Goldberg, answering questions about what the study found.
ConvergenceRI: Why did you conduct the study?
GOLDBERG: In the beginning of the COVID pandemic, we were struggling to find ways to diagnose and treat COVID. One of my colleagues reached out to me and asked if I’d like Lifespan emergency department hospitals [Rhode Island Hospital, The Miriam Hospital, Newport Hospital, and Hasbro Children’s Hospital] to be included in a new registry of COVID cases.
The idea was that if we could get multiple researchers to contribute data from their hospital sites, we could learn more about how to diagnose and treat our patients who were arriving in droves with this new, still poorly described infection. Ultimately, we were able to include 86 emergency departments in 27 states [from across the U.S.].
Soon thereafter, we started to realize that older adults were having higher rates of serious illness from COVID, and being both an emergency medicine doctor and a scientist interested in improving health for older adults, I wanted to know whether we were truly seeing worse outcomes for older people across the United States – and why?
In my clinical practice, I was starting to notice that older people were less likely to have “classic” symptoms of COVID. This made me worry that [older people] were flying under the radar [screen] and not getting treatment in a timely fashion. So, we decided to conduct a study to see if the data backed this up.
ConvergenceRI: What did you find?
GOLDBERG: We found that older adults, 65+, really did have unique ways they presented to the emergency department. Unlike younger people, they were less likely to have a cough, fever, and report loss of taste and smell.
For instance, while 29 percent of younger patients, aged 18-64, said they had ear, nose, and throat [ENT] symptoms, only 10 percent of adults older than 74 reported such symptoms.
Those ENT symptoms often served as big tip offs to us clinicians early on that the patient may have had COVID, when testing was scarce and turnaround times were abysmal. Older people did often complain of shortness of breath, but a lot of conditions can cause you to feel winded – such as heart failure, pneumonia, and heart attacks.
Older people also were more likely to have neurological symptoms such as confusion [2 percent of younger people presented confused, while 11 percent of those 65-74 and 26 percent of those 75+ had confusion].
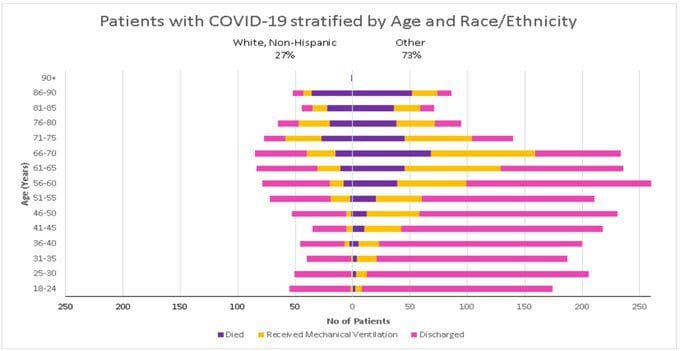
We found that older adults also had more severe disease that required an ICU stay or being placed on a ventilator, especially Hispanic or Black folks. We believe these disparities had to do with greater housing density, differences in access to resources, and structural racism.
We didn’t find that atypical symptoms and delays in diagnosis were the reason older adults had more severe illness. It turns out people with less typical COVID symptoms [cough, fever, shortness of breath] actually had better outcomes.
Several mechanisms could explain why older people have more severe disease. The immune response gets less robust when we age, termed “immunosenescence.” Older adults are more likely to have chronic inflammatory states due to dementia or other diseases.
There can also be less aggressive treatment due to age bias or advanced directives. And, we know many older people avoided the emergency department during COVID.
ConvergenceRI: Why were the study’s findings important?
GOLDBERG: The study is the largest study to date comparing emergency department presentations in younger and older people. Our findings showed that we really need to be cautious about relying on a symptom-only strategy to diagnose older people with COVID. It confirms that we need to be aggressive with testing even people that we think may not have COVID.
We now have antiviral drugs and monoclonal antibody treatments that we can use to reduce the severity of symptoms, if we diagnose COVID early or even prevent infection if you were exposed.
ConvergenceRI: How does the study suggest to you ways that we need to change our approaches to diagnosing COVID, moving forward?
GOLDBERG: This study adds to the literature that it is tricky to get the diagnosis right in older people. It’s harder to hone in on the diagnosis being an infection when a person comes in without fever, [because] older people often don’t mount the same high-grade fever response to infection that younger people do.
It also suggests that there isn’t “classic COVID.” You can have cough, fever, and loss of smell, but many people, especially older persons, will just feel weak, have new falls, or feel short of breath.
This study was done in a pre-vaccination cohort, so that is an important caveat. However, many Americans are still not vaccinated, and the study results are still relevant today, because testing is still not accessible and widely used by everyone who may be infected.
Also, new variants can partially evade vaccination and re-infection with different strains is possible.
[Editor’s Note: The authors of the study are:
• Dr. Elizabeth M. Goldberg, MD, ScM, Emergency Medicine, Brown University, Providence RI, USA
• Dr. Lauren T. Southerland, MD, Emergency Medicine, Ohio State University, Columbus, OH, USA
• Dr. Andrew C. Meltzer, MD, MS, Emergency Medicine, George Washington School of Medicine and Health Services, Washington, DC, USA
• Dr. Justine Pagenhardt, MD, Emergency Medicine, West Virginia University, Morgantown, WV, USA
• Dr. Ryan Hoopes, Alpert School of Medicine, Brown University, Providence, RI, USA
• Dr. Carlos A. Camargo, Jr., MD, Ph.D, Emergency Medicine, Massachusetts General Hospital, Harvard Medical School, Boston MA, USA
• Dr. Jeffrey A. Kline, MD, Emergency Medicine, Wayne State University, Detroit MI, USA]
_____
To read article in its entirety:
_____
To read more articles by Asinof, go to: https://rinewstoday.com/richard-asinof/

Richard Asinof is the founder and editor of ConvergenceRI, an online subscription newsletter offering news and analysis at the convergence of health, science, technology and innovation in Rhode Island.
To read more stories by Richard Asinof: https://rinewstoday.com/richard-asinof/
