Search Posts
Recent Posts
- Cranston Councilor Germain’s resignation charges get swift response, call for investigation April 18, 2024
- We Cook! Mill’s Tavern Short Rib Sage Polenta April 18, 2024
- Rhode Island Weather for April 18, 2024 – John Donnelly April 18, 2024
- Providence: A new culture in City Hall – Mayor Smiley’s FY25 Budget April 18, 2024
- RI Veterans: Did you know? 18.04.24 (100th bday, events, Q/A, fishing, resources) – John A. Cianci April 18, 2024
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.
What’s coming at us: 3,000 new cases a day. What do we do now? – Dr. Michael Fine
By Michael Fine
© Michael Fine 2022
Ok. More than 3000 tested positive cases on December 30, 2021. I just saw that the positivity rate of testing at one New York Hospital is fifty percent. Which is no surprise. With a doubling rate of three days, we likely have 6000 test positive cases by yesterday, January 2, 2022, if we tested 25,000 people. And 12,000 by January 5, 2022, which is about 50 percent positive. There is some bias implicit in testing: if you get sick you are more likely to be tested. Even so, I expected we are only a week away from 25,000 to 50,000 new cases a day. So likely a third of us or a half of us are going to get Omicron. As I’ve said before, I expect most schools, government offices, and businesses to have to close for a little while, just because they won’t have the staff they need to operate.
And I just ran some projections, which are daunting. Projections are just that – educated guesses. Mine are done on the back of an envelope, so take them with a grain of salt. You take the number of hospitalizations and deaths from October, November, and December, divide by the number of cases, and then multiply by the number of cases you expect. With Omicron we are flying blind, because we don’t know what portion of people who get infected end up in the hospital or dying. Many people think Omicron will cause less hospitalizations and deaths than Delta did, as a percentage of who is infected, which is a good thing. But there will be many more people infected which may cancel out the effect of Omicron being less virulent, so we may not see causing less hospitalizations and death even if Omicron is less virulent after all.
If you assume that Omicron is half as likely to cause hospitalization and death and you assume we never get beyond 3000 new cases per day (that number is likely to get much larger –fast), we must anticipate 168 deaths and 1745 hospitalizations in January alone, the most conservative set of assumptions. If you assume we average 10,000 new cases a day and Omicron having half the virulence of Delta, we must anticipate 613 deaths and 6205 hospitalizations in January. And so forth. If Omicron is only one forth the virulence as Delta, those numbers drop in half. If Omicron is as virulent as Delta, the numbers double. I just don’t know the real number, but I suspect the numbers will be close to the higher estimate, if not higher. I’m sorry to be the bearer of such bad news.
So, what should we do as a state, and what should be do as individuals?
As a state, we have to admit to ourselves that the horse is out of the barn, that the Maginot Line has been breached, although, because we didn’t require masks and continued to keep bars and restaurants open, we really never had a Maginot line. It is also now too late for more vaccination alone to prevent the rapid spread of the Omicron variant of Covid-19. From a public health perspective, that means we have to move from the prevention of community spread, which has failed, to harm reduction, to preventing the deaths still preventable.
The people at greatest risk continue to be the elderly and those with chronic disease. 55 percent of our deaths have been in people over 80; 78 percent of our deaths have been in people over 70; and 91 percent of our deaths have been in people over 60, with about 75 percent of our deaths in the last three months in people over 60, because of the number of deaths in younger, unvaccinated people. We can and should keep vaccinating the unvaccinated and boosting those at greatest risk as quickly as we can, but we’ve pretty much run out of time for vaccination – one week from today, by January 8, at least 24,000 are likely to be infected; by January 11, that’s likely to be at least 50,000 people. (The vaccine reduces the risk of hospitalization and death, at least in people under eighty, which is a good thing. But it is not yet clear how much the vaccine protects people over eighty or for how long that protection lasts. If Covid vaccines are like flu vaccines, that protection likely lasts only two months, and many people of that age got boosted in September, October, and early November. A recent report from the UK shows that protection against Omicron wanes more quickly than against Delta. After a third dose the Pfizer vaccine has initial 70% effectiveness against symptomatic infection, which declines to only 35% after 10 weeks. A Moderna booster has 75% initial effectiveness against symptomatic infection, declining to 45% by 10 weeks.)
BUT we should stop testing so many people. And stop contact tracing. We use testing to understand the level of community spread in a population and use what we know to intervene with contact tracing, isolation and quarantine, and other population-based interventions like masking and the closure of infected workplaces, schools, and businesses, most of which went ignored in Rhode Island. But none of that matters now – we know community transmission is extremely high everywhere in the state already, so we don’t need more testing to tell us what we already know.
We don’t have the resources we need to do meaningful contact tracing once we get much beyond fifty new cases per day – and we are over 3000. We should use all the monoclonal antibody we can get our hands on, and the antiviral drugs Paxlovid and molnupiravir, the new oral drugs, one of which is very effective against Omicron, and we should test only those people who meet criteria for monoclonal antibody administration or anti-viral medications– people over 65 with symptoms and those with significant chronic disease. It’s just dumb to have those people wait outside, in the cold, for four hours to get tested, because Omicron is so transmissible that we are likely spreading the disease by having people wait in those lines, even outside and masked. Instead, we need a few hundred monoclonal antibody and antiviral flying squads made up of the people who were doing testing and contact tracing, and the Rhode Island National Guard, in groups of two that can go to the houses of people at high risk who are symptomatic, rapid and PCR test them and get them started on MAB or antivirals right then and there.
And we should do point-of-entry rapid testing for anyone who wants to enter a public space. That way we know that people who are congregating aren’t likely to be shedding virus when they are together. We’ll need all sorts of people deployed to staff such a process. Which means we need to start organizing rapid testing on entry as soon as possible.
Then, we need to sequester the elderly and those with chronic disease so they don’t go out or get exposed to other people until the level of community transmission drops, which means we need to get them food and connection, calling often, facetiming when we can, so the isolation doesn’t drive them crazy. And we need to do our level best to keep those at-risk people safe, flattening the curve any way we can, until we get supplies of monoclonal antibodies that work against Delta and Omicron and antiviral therapies, which can be used to protect the vulnerable against hospitalization and death should they become infected, which, unfortunately, many of them will.
We need to support workers who can’t work and businesses that can’t operate financially during this period, so we don’t get trapped into the same cycle of people feeling like they need to go out to work so they don’t get evicted or go bankrupt.
It won’t be long this time – 6 to 8 weeks at max, so we shouldn’t overdo it. But we can’t leave anyone out.
And we need to find some way to support the amazing frontline health care workers, on whose backs this has fallen again. The state needs to call up everyone who has a license and isn’t working to help. And yes, please bake cookies again, and applaud them at shift change. It is small consolation for what we have all allowed to happen again, but small consolation is better than no consolation. And they, and we, need to remember, so we don’t get fooled again.
Everyone who has symptoms should isolate FOR TEN DAYS, after talking to their own doctor to make sure they don’t have something else that isn’t Covid. No testing needed. For the half of us that don’t have a family doctor, we need an 800 number staffed by clinicians working at home who can listen to them and make recommendations over the phone. And get them an out of work note. (BEAT COVID-19 in Pawtucket and Central Falls built an 800 number like that in two weeks in April of 2020. We need to wake that up asap and expand it so it can handle 20,000 calls a day or more, which is what is coming at us.) Everyone who is a contact should quarantine for at least seven, and preferably ten days. But that means most Rhode Islanders will be home for two weeks, you might say, once you’ve done the math. Yup. That’s exactly the point. It’s the only way we can whip this, the only way we can reduce the number of hospitalizations and deaths now. Sorry.
Every Rhode Island household needs a pulse oximeter. They cost less than $10 each, bought in bulk, and are the best tool a clinician over the phone has to assess how safe a person with symptoms is to stay at home. (Thanks to Anne Grant in Pawtucket for reminding me about this).
And then, come February or March, when the infections have stopped and the hospitals have emptied, we need to remember. There may be another variant. There will be another pandemic. We need to choose leaders who will put the public’s health in front of commerce, because, as I fear the next few weeks will show, if you don’t do that you don’t get either.
Yes, I’ve let people in state government know these ideas. I did that last week, before I saw Thursday’s numbers and heard about the hospital in New York that was running fifty percent positive tests. But government is what government is. It moves slowly. And this virus moves as fast a lightening. It is outrunning and outsmarting government at every turn.
So now it’s your turn. If you want this stuff to happen, pick up the phone. Call your mayor or your state senator or your state rep. (Don’t call the Governor. He’s got his hands full right now. I promise.) Mayors, state senators and state reps are the people who can put a fire under government to get this stuff moving. Remember the power in government actually is in yourhands. You have tremendous power if you raise those hands up and raise your voice up, together with your neighbors, all at the same time.
That’s what democracy looks like.
Thanks for reading. Please don’t sit on your hands. Stay safe. And happy new year.
Michael Fine M.D.
Many thanks again to Nick Landekic, who provided me with tons of data and publications over the last twenty months, and whose knowledge of Covid-19 is encyclopedic; to Deborah Faith, MPH, for her unending editorial support and great editorial suggestions, and to Kendra Tanquay, for her support of my writing over many months.
_____
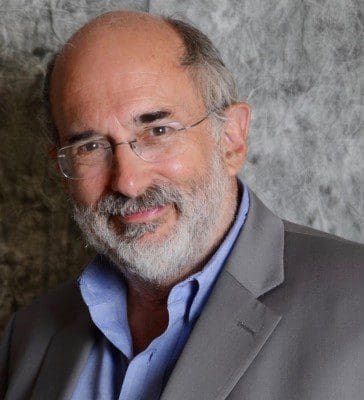
Michael Fine, MD was the Director of the Rhode Island Department of Health from February of 2011 until March of 2015. His career has been devoted to healthcare reform and the care of under-served populations. He served as Medical Program Director at the Rhode Island Department of Corrections; and founder and Managing Director of HealthAccessRI, the nation’s first statewide organization making prepaid, reduced fee-for-service primary care available to people without employer-provided health insurance.
Dr. Fine practiced for 16 years in urban Pawtucket, and rural Scituate, RI. He is the former Physician Operating Officer of Hillside Avenue Family and Community Medicine, the former Physician-in-Chief of the Rhode Island and Miriam Hospitals’ Departments of Family and Community Medicine. He was co-chair of the Allied Advocacy Group for Integrated Primary Care.
He currently serves on the Boards of Crossroads Rhode Island, the state’s largest service organization for the homeless, the Lown Institute, the George Wiley Center, and RICARES. Dr. Fine founded the Scituate Health Alliance.
Dr. Fine is past President of the Rhode Island Academy of Family Physicians, has served on a number of legislative committees for the RI General Assembly, chaired the Primary Care Advisory Committee for the RIDOH, and sat on both the Urban Family Medicine Task Force of the American Academy of Family Physicians and the National Advisory Council to the National Health Services Corps.
