Search Posts
Recent Posts
- Detailing Manhattan: Christopher Gray’s Legacy – David Brussat April 26, 2024
- Business Beat: BankNewport supports Kids’ Zone at new Save The Bay Hamilton Family Aquarium April 26, 2024
- Rhode Island Weather for April 26, 2024 – John Donnelly April 26, 2024
- GriefSPEAK: Dread. Fear. Welcome relief. – Mari Nardolillo Dias April 26, 2024
- Outdoors in RI: big animals, tiny Ticks, huge Trout, Chepachet’s Harmony Railway, 2A – Jeff Gross April 26, 2024
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.
NEW: Pfizer antiviral pill, Paxlovid, showing 88% reduced risk of hospitalization/death if taken within 5 days of first symptom
Pfizer today announced final results from an analysis of all 2,246 adults enrolled in its Phase 2/3 EPIC-HR (Evaluation of Protease Inhibition for COVID-19 in High-Risk Patients) trial of its novel COVID-19 oral antiviral candidate PAXLOVID™ (nirmatrelvir [PF-07321332] tablets and ritonavir tablets). These results were consistent with the interim analysis announced in November 2021, showing PAXLOVID significantly reduced the risk of hospitalization or death for any cause by 89% compared to placebo in non-hospitalized, high-risk adult patients with COVID-19 treated within three days of symptom onset.
In a secondary endpoint, PAXLOVID reduced the risk of hospitalization or death for any cause by 88% compared to placebo in patients treated within five days of symptom onset, an increase from the 85% observed in the interim analysis. The EPIC-HR data have been shared with the U.S. Food and Drug Administration (FDA) as part of an ongoing rolling submission for Emergency Use Authorization).
“This news provides further corroboration that our oral antiviral candidate, if authorized or approved, could have a meaningful impact on the lives of many, as the data further support the efficacy of PAXLOVID in reducing hospitalization and death and show a substantial decrease in viral load. This underscores the treatment candidate’s potential to save the lives of patients around the world,” said Albert Bourla, Chairman and Chief Executive Officer, Pfizer. “Emerging variants of concern, like Omicron, have exacerbated the need for accessible treatment options for those who contract the virus, and we are confident that, if authorized or approved, this potential treatment could be a critical tool to help quell the pandemic.”
EPIC-HR Final Results
In the final analysis of the primary endpoint from all patients enrolled in EPIC-HR, an 89% reduction in COVID-19-related hospitalization or death from any cause compared to placebo in patients treated within three days of symptom onset was observed, consistent with the interim analysis. In addition, a consistent safety profile was observed.
0.7% of patients who received PAXLOVID were hospitalized through Day 28 following randomization (5/697 hospitalized with no deaths), compared to 6.5% of patients who received placebo and were hospitalized or died (44/682 hospitalized with 9 subsequent deaths). The statistical significance of these results was high (p<0.0001). In a secondary endpoint, PAXLOVID reduced the risk of hospitalization or death for any cause by 88% compared to placebo in patients treated within five days of symptom onset; 0.8% of patients who received PAXLOVID were hospitalized or died through Day 28 following randomization (8/1039 hospitalized with no deaths), compared to 6.3% of patients who received placebo (66/1046 hospitalized with 12 subsequent deaths), with high statistical significance (p<0.0001). Relative risk reduction was 94% in patients 65 years of age or older, one of the populations at highest risk for hospitalization or death; 1.1% of patients who received PAXLOVID were hospitalized through Day 28 (1/94 hospitalized with no deaths), compared to 16.3% of patients who received placebo (16/98 hospitalized with 6 deaths), with high statistical significance (p<0.0001). In the overall study population through Day 28, no deaths were reported in patients who received PAXLOVID as compared to 12 (1.2%) deaths in patients who received placebo.
In the EPIC-HR trial, in a secondary endpoint, SARS-CoV-2 viral load at baseline and Day 5 have been evaluated for 499 patients. After accounting for baseline viral load, geographic region, and serology status, PAXLOVID reduced viral load by approximately 10-fold, or 0.93 log10 copies/mL, relative to placebo, indicating robust activity against SARS-CoV-2 and representing the strongest viral load reduction reported to date for an oral COVID-19 agent.
Treatment-emergent adverse events were comparable between PAXLOVID (23%) and placebo (24%), most of which were mild in intensity. Fewer serious adverse events (1.6% vs. 6.6%) and discontinuation of study drug due to adverse events (2.1% vs. 4.2%) were observed in patients dosed with PAXLOVID, compared to placebo, respectively.
(NCT04960202), were not yet available for this review. Full study data are expected to be released later this month and submitted to a peer-reviewed publication.
EPIC-SR Interim Results
Interim analyses of the EPIC-SR (Evaluation of Protease Inhibition for COVID-19 in Standard-Risk Patients) Phase 2/3 study, which included unvaccinated adults who were at standard risk (i.e., low risk of hospitalization or death) as well as vaccinated adults who had one or more risk factors for progressing to severe illness, showed that the novel primary endpoint of self-reported, sustained alleviation of all symptoms for four consecutive days, as compared to placebo, was not met.
The key secondary endpoint showed a 70% reduction in hospitalization and no deaths in the treated population for any cause compared to placebo. Additionally, there was approximately a 10-fold, or 1 log10 copies/mL, decrease in viral load compared to placebo, consistent with results from the Phase 2/3 EPIC-HR study.
The data were reviewed by an independent Data Monitoring Committee (DMC) and, based on the totality of the data available, the DMC recommended that the trial continue.
At the EPIC-SR interim analysis, which included 45% of the trial’s planned enrollment, 0.6% of those who received PAXLOVID were hospitalized following randomization (2/333 hospitalized with no deaths), compared to 2.4% of patients who received placebo and were hospitalized or died (8/329 hospitalized with no deaths). A follow-on analysis at 80% of enrolled patients was consistent with these findings. In this analysis, 0.7% of those who received PAXLOVID were hospitalized following randomization (3/428 hospitalized with no deaths), compared to 2.4% of patients who received placebo and were hospitalized or died (10/426 hospitalized with no deaths); p=0.051.
Treatment-emergent adverse events were comparable between PAXLOVID (22%) and placebo (21%), most of which were mild in intensity. Rates of serious adverse events (1.4% vs. 1.9%) and discontinuation of study drug due to adverse events (2.1% vs. 1.2%) were also comparable between PAXLOVID and placebo.
(NCT05011513), were not yet available for this review. The study is now fully enrolled, and further data will be released upon analysis of the full study data expected later this month.
About PAXLOVID™ (nirmatrelvir [PF-07321332] tablets and ritonavir tablets)
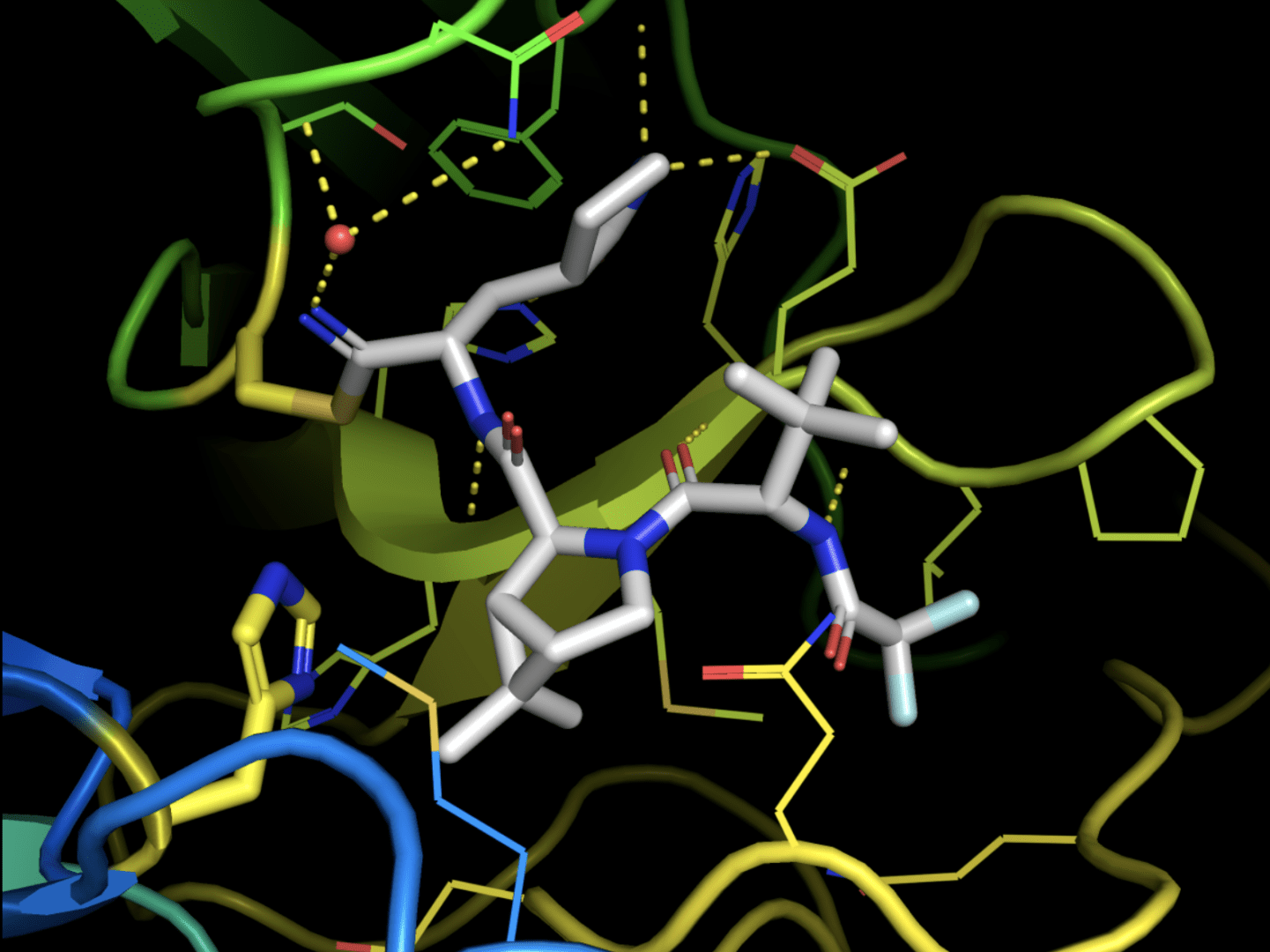
PAXLOVID is an investigational SARS-CoV-2 protease inhibitor antiviral therapy. It was developed to be administered orally so that, if authorized or approved, it can be prescribed at the first sign of infection or at first awareness of an exposure – potentially helping patients avoid severe illness (which can lead to hospitalization and death) or avoid disease development following contact with a household member who contracts COVID-19 – subject to the clinical success of the rest of the EPIC development program. Nirmatrelvir [PF-07321332], which originated in Pfizer laboratories, is designed to block the activity of the SARS-CoV-2-3CL protease, an enzyme that the coronavirus needs to replicate. Co-administration with a low dose of ritonavir helps slow the metabolism, or breakdown, of nirmatrelvir in order for it to remain active in the body for longer periods of time at higher concentrations to help combat the virus.
Nirmatrelvir is designed to inhibit viral replication at a stage known as proteolysis, which occurs before viral RNA replication. In preclinical studies, nirmatrelvir did not demonstrate evidence of mutagenic DNA interactions.
Current variants of concern can be resistant to treatments that are focused on the spike protein expressed on the surface of the SARS-CoV-2 virus, due to the mutations in this region. PAXLOVID, however, works intracellularly on the protease of the SARS-CoV-2 virus by inhibiting viral replication. Nirmatrelvir has shown consistent in vitro antiviral activity against the previously identified variants of concerns (i.e., alpha, beta, delta, gamma, lambda, and mu). In addition, nirmatrelvir potently inhibited the 3CL protease associated with Omicron in an in vitro biochemical assay. This indicates nirmatrelvir’s potential to maintain robust antiviral activity against Omicron. Additional in vitro antiviral studies with this variant are underway.
If authorized or approved, PAXLOVID will be administered at a dose of 300 mg (two 150 mg tablets) of nirmatrelvir with one 100 mg tablet of ritonavir, given twice-daily for five days. One box contains five blister packs of PAXLOVID, as co-packaged nirmatrelvir tablets with ritonavir tablets, providing all required doses for a full five-day treatment course.
About the Phase 2/3 EPIC-HR Study Top-Line Results
The final analysis of the primary endpoint evaluated data from 2,246 adults who were enrolled by November 4, 2021. At the time of the decision to stop recruiting patients, enrollment was at 75% of the 3,000 planned patients from clinical trial sites across North and South America, Europe, Africa, and Asia, with 41% of patients located in the United States. Enrolled individuals had a laboratory-confirmed diagnosis of mild to moderate SARS-CoV-2 infection within a five-day period and were required to have at least one characteristic or underlying medical condition associated with an increased risk of developing severe illness from COVID-19. Each patient was randomized (1:1) to receive PAXLOVID or placebo orally every 12 hours for five days.
About the Phase 2/3 EPIC-SR Study Interim Analyses
The primary analysis of the interim data, consisting of the first 45% of patients enrolled in the study, included 673 adults, of whom 338 received PAXLOVID and 335 received placebo. At the time of the interim analyses, EPIC-SR had reached its planned enrollment of more than 1,140 adults from clinical trial sites across North and South America, Europe, Africa, and Asia, and the United States. Enrolled individuals had a laboratory-confirmed diagnosis of mild to moderate SARS-CoV-2 infection within a five-day period and were either unvaccinated adults who were at standard risk (i.e., low risk of hospitalization or death) or vaccinated adults who had one or more risk factors for progressing to severe illness from COVID-19. Each patient was randomized (1:1) to receive PAXLOVID or placebo orally every 12 hours for five days.
About the EPIC Development Program
The EPIC (Evaluation of Protease Inhibition for COVID-19) Phase 2/3 development program for nirmatrelvir; ritonavir consists of three clinical trials spanning a broad spectrum of patients, including adults who have been exposed to the virus through household contacts, as well as adults at both standard risk and high risk of progressing to severe illness.
In July 2021, Pfizer initiated the first of these trials, known as EPIC-HR (Evaluation of Protease Inhibition for COVID-19 in High-Risk Patients), a randomized, double-blind study of non-hospitalized adult patients with COVID-19, who are at high risk of progressing to severe illness. At the recommendation of an independent Data Monitoring Committee and in consultation with the U.S. Food and Drug Administration (FDA), Pfizer ceased further enrollment into the study in early November 2021 due to the overwhelming efficacy demonstrated in results from an interim analysis. Data have been submitted to the FDA as part of its submission for Emergency Use Authorization, and findings from the EPIC-HR interim analysis have been submitted to a peer-reviewed journal for publication.
In August 2021, Pfizer began the Phase 2/3 EPIC-SR (Evaluation of Protease Inhibition for COVID-19 in Standard-Risk Patients), to evaluate efficacy and safety in patients with a confirmed diagnosis of SARS-CoV-2 infection who are at standard risk (i.e., low risk of hospitalization or death).
In September, Pfizer initiated the Phase 2/3 EPIC-PEP (Evaluation of Protease Inhibition for COVID-19 in Post-Exposure Prophylaxis) to evaluate efficacy and safety in adults exposed to SARS-CoV-2 by a household member. This trial is ongoing.
Top graphic: Xray crystal structure of the SARS-CoV-2 protease inhibitor PF-07321332 bound to the viral protease enzyme. Ribbon diagram of the protein with the drug shown as sticks. The catalytic residues are shown as yellow sticks.
.
