Search Posts
Recent Posts
- It is what it is – Jen Brien April 24, 2024
- Time for Sour Grapes – Tim Jones April 24, 2024
- Tenor and Pianist, Michael DiMucci: Songs From the Heart at Linden Place Mansion April 24, 2024
- World War II Veteran, Louis Dolce, turns 100 – TODAY April 24, 2024
- Rhode Island Weather for April 24, 2024 – John Donnelly April 24, 2024
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.

Hospital Emergency Department crisis puts onus on patients to know when not to go.
Don’t go to the Emergency Room. Go elsewhere. Unless you need full emergency care. That was the bottom line delivered by Dr. Alexander-Scott from the RI Department of Health as emergency rooms and hospitals, in general, are experiencing an emergency of their own in staffing and capacity.
In a press conference rescheduled to take place outdoors, the Health Department released a statement; a summary is printed here:
In advance of holiday gatherings and the height of flu season in Rhode Island, State health and hospital officials gathered today to again urge the public to only go to emergency departments for health issues that require emergency care. Hospital emergency departments in Rhode Island continue to experience significant crowding and prolonged waiting times.
Many health issues can be treated quickly and effectively by a primary care provider or in an urgent care facility. This includes less severe cases of the flu, back pain, minor cuts, sore throats, low-grade fevers, and most cases of norovirus (the “stomach flu”). Patients will experience long wait times in the emergency department for non-urgent symptoms or may board there for a significant period before hospital admission.
“Emergency departments are perfect for emergency situations. If someone is experiencing a serious health issue, they should absolutely call 911 or go to an emergency department right away. However, emergency departments treat patients with the most serious health issues first, which means that people with less severe conditions will experience long waits,” said Director of Health Nicole Alexander-Scott, MD, MPH. “Keep the phone number for your primary care provider handy and know where your nearest urgent care facility is. An urgent care facility, or other type of express care facility is often a more convenient, less expensive option.”
A new resource for patients to reference when they think they need immediate care has been developed and is on their website: health.ri.gov/rightplacerightcare. This new page has links to lists of primary care providers, urgent care centers, and health centers in Rhode Island, and guidance on when and when not to go to the emergency department. The page also links to a page of primary care doctors.
“In working with our health systems in Rhode Island, it has become abundantly clear that hospital overcrowding has emerged as a priority concern for the state,” said Executive Office of Health & Human Services Assistant Secretary Ana Novais. “I am thankful for our interagency team that is reviewing these challenges, implementing some immediate relief, and planning strategies to address these issues long-term.”
They reinforced that the pandemic healthcare crisis is not over and both adult and pediatric EDs all around the country are experiencing staffing shortages. Behavioral health patients can be “boarded” for days waiting for appropriate placement.
_____
Where to go when there’s nowhere to go?
For those without insurance, or who are undocumented, or who have no funds to pay out of pocket at a private urgent care facility, true emergency care can only be had in a hospital.
For non-emergent treatment options:
Community Health Centers are listed as a resource – but only if you are already an established patient. You might consider becoming a regular patient with your nearby center, now, if you do not have a primary care physician, so you can have that disqualifier remedied.
Community Health Center Express Clinics are available in Pawtucket, Central Falls, Providence, Wakefield, West Warwick, and Woonsocket – while most are open 7 days, most area also not open 24/7.
CVS Minute Clinics have walk-ins, but not 24/7 in about 8 cities in RI.
No Insurance?
The RI Free Clinic is for adults only, but does take patients without insurance, though they are not open 24/7.
Clinica Esperanza notes patients who have no insurance have no option but to go to an emergency room for serious healthcare needs – they can’t go to urgent care centers which usually only accept insurance.
If you must seek emergency care at a hospital, the Health Department notes, “ask about the hospital ‘charity care’ program. The hospital may cover all or part of your bill if you are unable to pay. The hospital must post its charity care eligibility rules and how to apply. Ask the business office of the hospital for an application. Charity care is available regardless of immigration status. If you need to have emergency services at a hospital, and you are not eligible to enroll in Medicaid just because of your immigration status, you may be eligible to have Medicaid pay the hospital bills. The hospital helps you fill out the application.”
When to seek emergency care
If someone is showing any of these signs, seek emergency medical care immediately:
- Trouble breathing
- Persistent chest pain or chest pressure
- New weakness in an arm, leg, or face
- New difficulty speaking or confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone
If you are going to an emergency department for COVID-19-like illness, notify the facility that you (or the person you are accompanying) is seeking care for COVID-19. Masks are required in all healthcare facilities.
Measures being taken at the State level
An interagency team across the Executive Office of Health and Human Services (EOHHS) is working toward the development and implementation of strategies to address the challenges facing hospitals. They include:
- Emergency regulations to assist increase the workforce and pre-hospital transportation availability.
- Partnerships with urgent care centers to explore developing capacity to expand emergency treatment options.
- Development of step-down capacity for behavioral healthcare and increased treatment initiation within emergency room settings.
- Provision of staffing supports, including direct care workforce recruitment and retention initiatives for home and community-based services.
- Planning for mobile crisis response for behavioral health and increased behavioral health system capacity through Certified Community Behavioral Health Clinics.
Where’s the message to the primary care doctors’ practices?
Missing from the messaging at the Health Department today was an out-of-the box solution, or a suggestion involving the primary care and family doctors’ practices as integral in solving the problem, even in the short term.
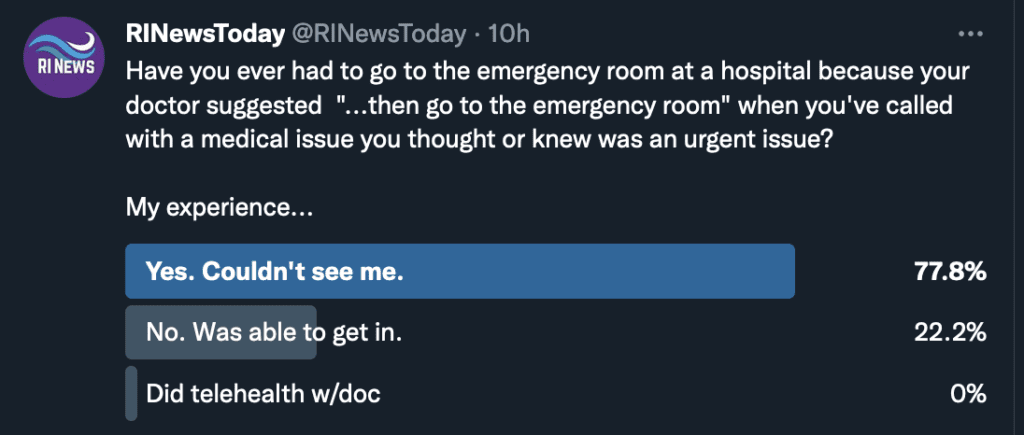
How often is it that a patient can be directed to “go to the emergency room” by their doctor because there are not any patient openings. We surveyed, informally, and asked our readers. This is their response – nearly 78% were directed to go to the emergency room by their primary care doctor’s office, not because they had been screened that they had a true medical crisis, but because they could not see the patient within a short period of time – leaving it up to the patient to decide what to do:
Some creative ideas utilized elsewhere:
The staffing crisis is not new to the pandemic. It existed in some degree prior to that. Often, “no ICU beds” really means no staff for those units. It is estimated that 1 in 5 medical professionals have left emergency medicine in the last two years. In August 1/2 million healthcare workers in this field left their jobs – in one month.
Other states are identifying unique ways of handling the crisis, which is a national one – and found a few operational changes that were making a difference, in addition to telling people not to use the emergency rooms unless absolutely necessary. Some are:
Primary cares add temporary end-of-day hours to treat patients with emergent issues during this crisis.
Behavioral health and mental health crisis response protocols – adults and children are using hospital emergency rooms because there are few services available to them in a true crisis, often occurring in evening hours and on weekends. “Boarding” for days or weeks while mental health beds open up somewhere – Butler Hospital or elsewhere – is increasing – are the mental health professionals at the table to solve the solution?
Some Massachusetts hospitals are using MedFlights to take patients to hospitals with open ICU units. Boston MedFlight provides transportation regardless of a patient’s ability to pay.
Hospitals co-locate General Practitioner clinics in all EDs to “decant”, or triage, non-emergency patients seeking care at the ED.
Improve Telehealth options in Rhode Island – the Health Dept. messaging didn’t mention Telehealth at all, which proved itself during the pandemic. It’s capacities can only be further utilized to problem solve this growing healthcare crisis. Note, in RI if you are insured by Blue Cross Blue Shield, they have an app you can download for their own Telehealth service. Again, not available 24/7.
In one study we reviewed, the importance of setting the overall vision for care during this time was reinforced. What is the Rhode Island vision for emergency medical care of our people?
While no system will ever likely reach the ideal, a suggested aspirational goal is, “Every person receives the right service in the right place, every time.”
