Search Posts
Recent Posts
- Writer Herb Weiss’ 45 years of Advocacy on Aging now Archived at Rhode Island College Library Special Collection June 23, 2025
- Providence Biopharma, Ocean Biomedical, Notified of Termination of License Agreements with Brown University, RI Hospital June 23, 2025
- Networking Pick of the Week: Early Birds at the East Bay Chamber, Warren, RI June 23, 2025
- Business Monday: Dealing with Black and White Thinking – Mary T. O’Sullivan June 23, 2025
- Rhode Island Weather for June 23, 2025 – Jack Donnelly June 23, 2025
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.
Dr. McDonald’s rules to live by: Love one another. Don’t be a jerk. COVID, year 3 – Richard Asinof
by Richard Asinof, ConvergenceRI, contributing writer
An in-depth interview with Dr. James McDonald, medical director at the R.I. Department of Health, as the battle against COVID enters its third year
From the moment when Rhode Island sounded the alarm on Feb. 28, 2020, about the presence of the first coronavirus case in the state, with the Governor’s news conference held in the basement auditorium at the R.I. Department of Health, the agency has been front-and-center in leading the public health fight against the pandemic.
In recent months, that role has often placed the agency in the crosshairs of pundits [and gabmeisters on WPRO such as Dan Yorke] for adhering to best practices when it comes to protecting the public: masking, testing, vaccinating, quarantining when necessary, all to protect the public against further spread of the virus.
The current tension between the agency and Gov. Dan McKee has become palpable, as the Governor has so far resisted efforts to enforce masking mandates and vaccination mandates, all the while touting his efforts to keep the economy on a pathway toward recovery, citing statistics from Moody’s.
Most recently, word reached ConvergenceRI that Gov. McKee is seeking to cut some 25 percent from the current budget for COVID-related activities at the R.I. Department of Health, according to a number of sources. That effort to cut the agency budget would seem to be ill-timed, given the rising number of cases and hospitalizations and the emergence of a new variant, omicron.
At the news conference held on Thursday afternoon, Dec. 9, by Gov. McKee and Lt. Gov. Sabina Matos, the Governor sidestepped the question by ConvergenceRI if he was seeking to cut the Health Department budget by some 25 percent, while, at the same time, he admitted that his administration was seeking to return to the budget of pre-COVID days.
The rest of the news media, however, fixated on whether the Governor was going to issue a mask mandate in response to increasing pressure from hospitals to do so, seemed to ignore and disregard the budget issue altogether. [If they can get you to keep asking the wrong questions, they don’t have to worry about the answers, as Thomas Pynchon once warned in Gravity’s Rainbow.]
[Editor’s Note: An announcement late on Friday evening by the Governor’s office seemed to indicate major changes in policy related to responses to COVID “containment” policies were afoot, slated to be announced early this week.
That was followed by the announcement by the Governor’s office on Saturday afternoon that the first case of the omicron variant had been identified in Rhode Island, including a message from Dr. Alexander-Scott, director of the R.I. Department of Health, urging Rhode Islanders to continue to protect themselves and their families through “vaccination, booster doses, mask wearing, testing, social distancing and ventilation.” Stay tuned; speed bumps ahead.]
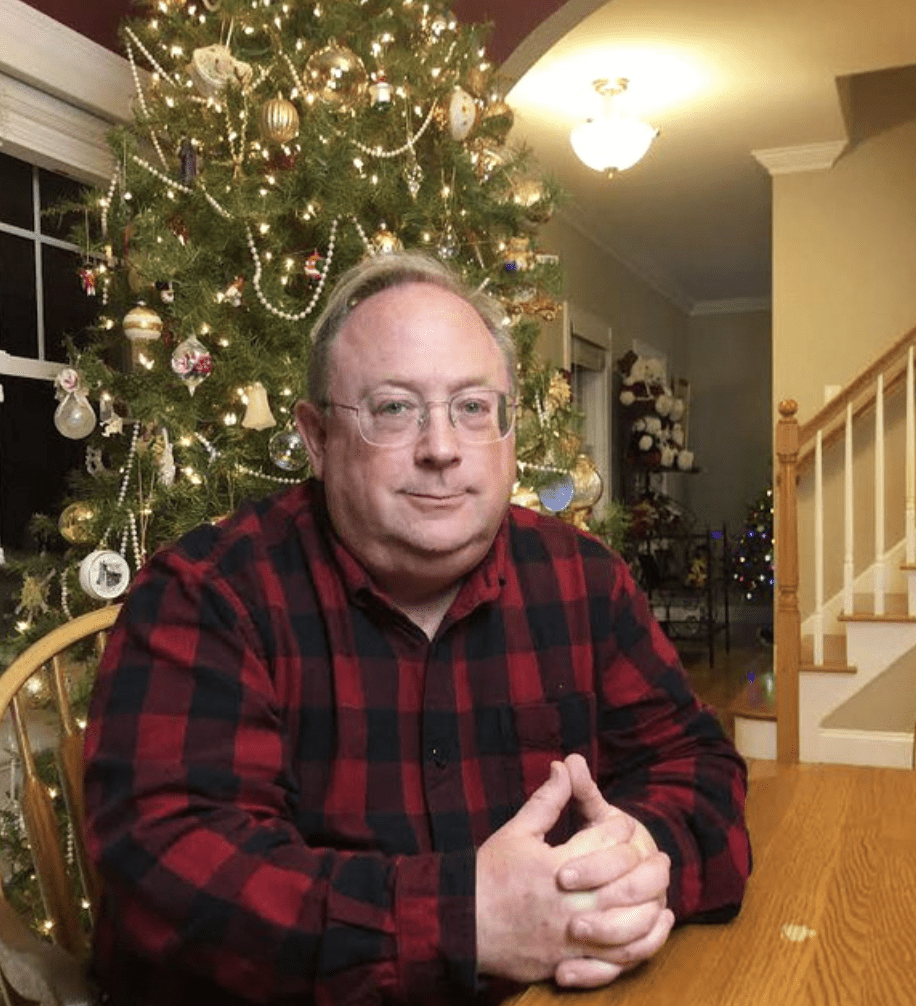
One of the truth-tellers at the R.I. Department of Health for the last two years has been Dr. James McDonald, the agency’s medical director, who has become a favorite of local TV networks for his avuncular style and his ability to explain what is happening in a folksy, Mr. Rodgers-in-the-neighborhood tone of voice.
But McDonald was all serious business when it came to talking about the ever-increasing demands that the coronavirus pandemic has placed on the agency – and upon all Rhode Islanders.
“Human beings aren’t used to things going on [and on],” McDonald told ConvergenceRI in a recent interview. “They are used to things starting and finishing. And, the pandemic is going to continue,” he warned. “This is a disease that is going to persist.”
In other words, McDonald continued, “It is not just that the disease will be pandemic, but that it [will become] a permanent disease.” That is not necessarily the truth-telling message that Gov. McKee wanted to hear, for sure.
At the same time, McDonald voiced an enduring optimism about the future, saying: “Everybody needs hope.” He shared the code that he says he lives by, in his down-to-earth communications style. “I have two rules of life that I live by. Rule Number One for Jim McDonald is: Love one another. Rule Number Two is: Don’t be a jerk.”
Here is the ConvergenceRI interview with Dr. James McDonald, as the state and the nation prepare to enter its third year in the battle with the coronavirus pandemic, providing a realistic assessment of where Rhode Island is – and where we need to go – with particular attention being paid by McDonald to the best strategies on how to counteract the forces of misinformation.
ConvergenceRI: I have heard that the Governor wants to cut 25 percent of your budget dealing with the response to COVID?
McDONALD: I have not heard that. But I am not traditionally involved with the money side of the Department. Other people would have heard that before I would.
ConvergenceRI: What is the current response to COVID, particularly now? How are things being organized? How important is the work that the Health Department is doing, work that may not get seen?
McDONALD: Let me start with this. You know, I think one of the things about the pandemic, as we approach the two-year mark, from Feb. 28, 2020, [of the first case in Rhode Island], is this: Human beings aren’t used to things going on; they are used to things starting and finishing. And, the pandemic is going to continue. This is a disease that is going to persist. In other words, it is not just that the disease will be a pandemic, but it [will become] a permanent disease.
One of the things that I think people forget is that before this was called SARS COV-2, it was called the “novel” coronavirus – and novel means new. What it really meant was that no human being on the planet had immunity.
What’s important about that is, even though we have vaccinated a lot of people, even though some people have immunity from natural infection, there are still a fair number of people who are not immune, so they are at risk.
On top of that, you have new variants [emerging]. We are dealing with omicron variant right now, but it is possible we will have to use something beside the Greek alphabet, because it only has so many letters.
My point is this: If we are going to manage this permanent disease from a public health standpoint, then we need to make sure that we have the funding and the infrastructure to do so. That will look different over time. But it is still going to require a pretty significant response from the R.I. Department of Health.
ConvergenceRI: Clearly, two years ago, I don’t think you ever anticipated that you were going to become a media star of sorts, appearing on television on a regular basis. How has the Health Department adapted to the new roles that it has to play?
McDONALD: I definitely did not anticipate being in the public eye. Just to make sure that is really clear to you. That only happened because the Director [Dr. Nicole Alexander-Scott] had a cold one day, and the other person was busy, and all of sudden, I was there.
What I think you are more interested in, though, is where do we see the Health Department going, really looking at the future.
ConvergenceRI: Yes. The Department is, in many ways, the public health army – or the public health team – that is often standing in between the health threats that are out there, and all of us. Most of the time, when people talk about public health, if you are doing a good job, you are not being seen. I think, with this pandemic, it is just the opposite. To be doing a good job, you have to be seen.
McDONALD: I think that is a good way of putting it. Let me give you another analogy that might make more sense.
We are used to the traditional doctor [or nurse] who takes care of the patient. And when the traditional physician takes care of the patient, we make certain assumptions. That is that the doctor has our best interests at mind, that the doctor knows us, and that the doctor is up to date on the best treatments or preventatives to a disease.
That is the traditional view of what being a doctor is. And, oh, by the way, we really like the fact that a doctor actually cares about us, knows us, and really wants to help us.
One of the things that I think the state of Rhode Island has seen is that the R.I. Department of Health is, in many ways, one of their doctors.
Because I think what they have seen about the R.I. Department of Health is: we actually do know a fair amount about you, about the people who live in our state. We are up to date on the latest science; we are up to date on the latest treatment and we are an objective voice that will give you the best information possible.
One of the things we also see, when people are looking at the Department of Health, especially during the pandemic, what people are looking for is: where can I find truth?
Because we’ve seen a fair amount of information that is, quite frankly, wrong, in various media circles. And, [people] would like to have a reliable place to find truth.
I think one of the things that people realize about this Department is not only is it a reliable place to find truth, but they understand that the Department actually cares about that. We understand that there are social determinants of health that really do influence everyone’s health.
We recognize that people really do need a safe place to live. You need a safe place to learn. You need reliable transportation. And, that sometimes services have to be tailored.
People keep on realizing that the Health Department is into population health, but they are also [serve] as one of their doctors – because they get reliable, expert advice from the Department of Health that they can count on.
They give it to me in a way that I can actually understand it, and I think that is one of those things that really helps the public, because when you really think about the general public, they are made up of individuals, and they are going to make their own individual decisions, and people like to be able to make their own choices, and decide what works for them.
But, if they don’t get reliable, trusted information, they either make the wrong decisions, or they don’t make any decision at all, which often is the same as making the wrong decision.
ConvergenceRI: That leads to my next question, which is: How do you combat disinformation and misinformation and things that are just plain factually wrong?
McDONALD: I have two rules of life that I live by. Rule Number One for Jim McDonald is: “Love one another.” Rule Number Two is: “Don’t be a jerk.”
I do care deeply about other people, and I have to be kind about it. Because, when you argue with people, you are often not persuading them, you are just elevating their emotions into a place that isn’t healthy for them, or for me.
What the Department has recognized is that this pandemic has shown that there has been a great deal of “organized disinformation.” Some of it [has to do] with different groups having agendas – that are self-serving to those groups.
What we have tried to do is not waste time attacking groups that are acting in their own interests. Instead, we try to make sure that we get the truth out, in as many ways possible, and let that objective truth stand on its own. And, whenever possible, explain the truth in a way that anybody can understand it.
And, I think one of the things that the Department has tried to do is to recognize that people receive information not just in different media forms, but they receive different messages. People are individuals, and not everyone receives information the same way.
ConvergenceRI: Can you explain what you mean by that?
McDONALD: We are trying to keep things culturally appropriate, recognizing that people have different cultural perspectives, also different educational levels, and different patterns of thinking. So, when you are giving information to people, you have to do it through the culture they live in. in the world they live, and try to do it in a way that makes the most sense to them, without offending them.
Because the Department is a positive organization; we are not interested in attacking anybody. We trying to put out positive, restorative information, to help us to heal from the trauma that we have been through. And then, people can make the best decisions possible.
ConvergenceRI: We are not only dealing with the coronavirus pandemic, but we are also dealing with opioid overdose epidemic. My question is: How do you get your voices heard? And, how can government change its relationship with providers that are community agencies, so that they are not seen just as vendors, but as partners?
McDONALD: I don’t know if Yogi Berra said this, but he might have. Ninety percent of public health is half [about] relationships. Rhode Island is a state that is small enough, where you can actually form relationships with people, and form relationships with policy leaders, and establish trust.
I think one of the things that the Department has been really good at is creating those community partnerships, where there are avenues for everyone to get involved. Whether it is through Health Equity Zones, the Governor’s Task Force [on Overdose Prevention and Intervention], or any number of the other advisory committees that are out there,
We are trying to be everybody’s Department of Health, where people can actually connect with people, and actually get their voice heard.
I think you are right. We are in a pandemic, but it is not just a pandemic; it is not just the overdose epidemic. It is not just the behavioral health crisis going on, it is not just the structural racism issues, it is all that taken together.
And that is contributing to what is going on during this pandemic. But if people don’t have anywhere to go where they can voice what they are experiencing during this pandemic, then that puts a lot of hopelessness into people.
When you think about the R.I. Department of Health, we are here for the long-term. We have hundreds of years of future in front of us; we are not going anywhere. And so, we have the time and the desire and the inclination to look at whatever long-term problems that can be solved.
If we are not willing to tackle the social determinants of health, we are not going to see sustainable changes in our culture. [Many of us] grew up in America, thinking that our children would have better lives than we had. I know my parents had that thought, and their parents had that thought.
One of the things I have seen with this generation that has made them a little more dystopian is that they no longer hold onto that belief, and if we are going to move our dystopian generation to one with any meaningful amount of optimism, it starts with being able to participate in public health, no matter who you are, and then it gets to a larger issues, which I think gets to how do we meaningfully address what are really social determinants of health.
And, addressing those issues [that occur] outside of the exam room, that actually do [have an] affect on everyone’s health outcomes. Because, if you don’t have transportation, if you can’t get a meaningful education, and you don’t have a safe neighborhood, we don’t have a lot of hope.
And, this gets back to another issue. If you look at a paper that came out recently, about adverse childhood experiences, [“Adverse Childhood Experiences and Long-Term Health among Adults in Rhode Island”] 16 percent of the population of the state reported having four or more ACEs events
Four or more adverse childhood experiences to 16 percent of the population – these are all preventable things, but it really gets to the point that if we want to have a better future for the next generation, we’ve got to stop having adverse childhood experiences, and if you want to stop adverse childhood experiences, you have got to do things so that families can succeed – like flexible work policies for families, like supports for families, like access to a decent education, like treatment for people with substance abuse issues, like meaningful health care for people who have anxiety and depression, so they can be treated appropriately in a timely manner. Those are just a few examples of ways to prevent adverse childhood experiences.
ConvergenceRI: How does the Department of Health get recognized for the expertise that you have? I reported this week on the dialogue between Sen. Josh Miller and outgoing R.I. Medicaid Director Ben Shaffer, in which Shaffer seemed to, in my opinion, discounting the value of legislative leaders attempts to enact new laws to increase Medicaid rates.
In recent years, I have observed that there is a tendency to elevate consulting group experts above the expertise of people working the field. I believe that may have happened during the initial response to COVID, when you had folks from the Boston Consulting Group and McKinsey & Co. come in and supersede the functions of agencies.
How do you change the perception to reinforce that it is the folks at the Health Department who have the expertise, and not the private consulting groups?
McDONALD: You are illustrating, to some degree, a generational and cultural phenomenon. A book I read recently is relevant here, it is a book by Dr. Tom Nichols called The Death of Expertise.
It speaks to the attack on science and the rise of confirmation bias. One of the things that I remember from the very early part of the pandemic, even before we had our first case here, is trying to understand how we were going to explain complex public health concepts to the Governor’s team.
I remember explaining to the Governor at the time: “We isolate the ill, and we quarantine the exposed.” It was one of the first times I spoke up in a meeting, and she liked that, because she could understand it. Even to this day, you still see people confusing isolation and quarantine. In public health, our job is to explain things to the public in a way that they can understand it.
However, what you find sometimes – and this is part of the cultural phenomenon – is that when people listen to subject matter experts from the Department of Health, many of whom have doctoral degrees and who are deep subject matter experts, and then they weigh that opinion next to [someone] who may have no expertise at all and who may just have a passing familiarity with whatever we are talking about, and, which, quite frankly, may be objectively wrong.
I think part of why the pandemic has perpetuated so much in the United States is because of that very issue. In other words, people in the United States are confused, because they think the opinion, quite frankly, of anybody is the same value as the opinion of a national expert.
And that comes from growing up with this notion that everyone has a right to be heard, which is true, but even though everyone has a right to be heard, it doesn’t mean everyone is right.
When my car doesn’t work, I really don’t care what my neighbor thinks is wrong with my car. I very much care about what my mechanic says is wrong with my car, because I want the darned thing fixed and working. I know to go to experts to get my problems fixed.
I think with public health, there was so much confusion. Because some people felt that they have done research, but really all they’ve done is read several web pages that told them what they wanted to believe. And that isn’t research; that is leisure reading.
One of the things that public health professionals can help navigate is convincing political leaders what is best path forward. Because make no mistake about it, in the United States, [the fight against] this pandemic has been led by elected officials, that is who has been making the decisions, it is the elected officials.
One likely source of the confusion is that the responses from the New England states look very, very different from some of the Southern states. That was very confusing to a lot of people, different government officials were making very different decisions. What is unfortunate about that is,people have died, because they didn’t listen to public health experts, and that is just tragic. And, quite frankly, it was avoidable.
ConvergenceRI: Moving forward, what would you like to see happen?
McDONALD: I think people have to stop saying that they are tired of the pandemic. It is sort of childish, because the pandemic is here to stay, and it is not going away. One of the things we have to acknowledge is that the pandemic is here for as long as it is going to be here. And, since it is going to be here for a long time, we need sustainable strategies that will help us beat the pandemic. Not just in this state, not just in the country, but across the planet.
Right now, we are set up to be on this perpetuating cycle of variant after variant. In other words, globally, we can’t seem to get our act together. Globally, what we need to do is to have mass global production of a meaningful vaccine.
And, to get enough people vaccinated globally so that we can get this thing to come to an end. That is a global problem. It is unfortunate that we see affluent countries struggling to convince people to get a booster vaccine, when there are plenty of countries that are struggling to get one vaccine dose into high-risk individuals. So, I think global disparity is a big problem.
I think locally, we need to look at what are the mitigation measures that make sense. One mitigation measure is getting 80 percent or more of our population to get a booster vaccine in our state.
Another mitigation measure that doesn’t cost a lot of money and isn’t really all that hard is making sure that people wear masks when they are outside of their home when they are inside a building. Boosting and masking are two tangible things that would help us in the short term.
What you are going to see happen, I believe this week is, you are going to see more cases per day this week than there was one year ago. Although that is concerning, you are not going to see more hospitalizations than we saw one year ago. Or more deaths, because we have a vaccine. And, we have monoclonal antibodies.
ConvergenceRI: What haven’t I asked you, should I have asked you, that you would likle to talk about?
McDONALD: I’ll end with something philosophical. Everybody needs hope, and it is kind of corny, but our state’s slogan is hope, and there is something powerful about hope.
When you look at public health, public health is really about allowing everybody to have a decent life chance. It is public health, not political health. Public health is really about protecting and helping everyone.
If you have a healthy Health Department, you are more likely to have a healthy state. We need to make sure that the Health Department is free from political influence and that it has the tools it needs to succeed.
_____
To read complete story go to: http://newsletter.convergenceri.com/stories/it-is-all-about-public-health-not-political-health,6957
To read more articles by Richard Asinof, go to: https://rinewstoday.com/richard-asinof/
_____

Richard Asinof is the founder and editor of ConvergenceRI, an online subscription newsletter offering news and analysis at the convergence of health, science, technology and innovation in Rhode Island.
