Search Posts
Recent Posts
- Rhode Island Weather for May 31, 2025 – Jack Donnelly May 31, 2025
- Burn with Kearns: Fix Your Foundation: Core, Mobility & Joint Health – Kevin Kearns May 31, 2025
- In the News… quick recap of the week’s news (5.31.25) May 31, 2025
- Business Beat: Navigant CU receives prestigious Community Impact Award from NEACH May 31, 2025
- To Do in RI: Taste of Rhode Island. Food, libations, entertainment, auction for Matunuck Oyster Bar May 31, 2025
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.
Trouble ahead, trouble behind…
By Dr. Peter Simon, for Richard Asinof, ConvergenceRI.com
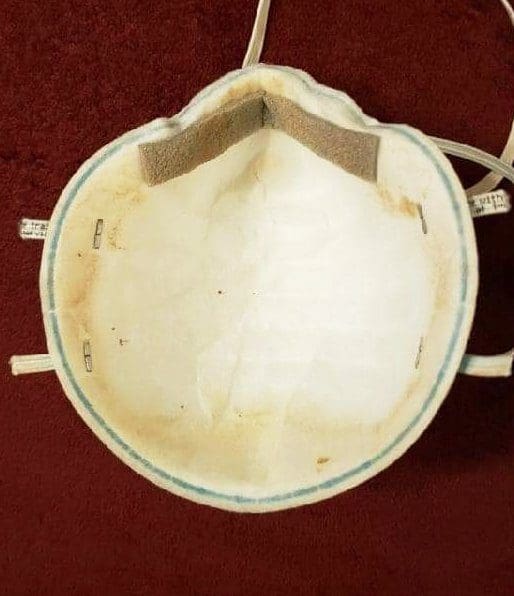
Photo: “This is an actual ‘decontaminated’ N95 mask that Albany Medical Center gave a nurse to use,” as tweeted out on Friday, Oct. 23, by Pat Kane. In response, Dr. Megan Ranney, an emergency room physician in Rhode Island, responded: “I have no words for how wrong this is, and how angry it makes me.” Ranney, who has set up a nonprofit, get usppe.org, continued: “I dare you to suggest that this mask still has structural integrity and can protect this nurse. We are the United States. Our frontline workers deserve better than this.” The reality is that as Rhode Island and the nation enters a new surge of coronavirus cases, hospitalizations and deaths, the lack of personal protection equipment, or PPE, continues to be a major problem, threatening the health and well-being of nurses, doctors and patients. Pat Kane’s Twitter Feed
Those with “power” and “money” have determined the shape of our health system. Without a shared understanding of the burden of disease and threats to the health of the people of Rhode Island – and their experiences seeking care in the present time, we may not see much changing for the good for us all in the future, following the coronavirus pandemic.
What we know and what we need to know
Off the coast of Greece, there are several island communities where residents routinely experience good health into their 10th decade. Researchers for decades have set up shop on these islands to observe and measure the patterns of living to see what are the elements that contribute to these healthy outcomes.
I know there are five determinants often cited from this work: genetics, behavior, environmental and physical influences, medical care and social factors.
How many of these five interconnected determinants have been discussed as part of the future long-term planning for health in Rhode Island? For instance, what are the projected health costs for rebuilding the Route 6/10 Connector in terms of future chronic disease burdens on the communities surrounding the highway?
Longitudinal design
When looking for the causes of risk, disease or any adverse outcome, I was taught by Dr. George Comsock, my professor of Epidemiology at Johns Hopkins University School of Hygiene and Public Health, many research designs are available but none can compare to longitudinal design.
One study that meets such criteria that many will recognize is the Framingham Heart Study. Can anyone name another similar study in the U.S.? Or, here in Rhode Island? The ongoing research by Professor Anna Aizer, chair of the Economics Department at Brown University, looking at the longitudinal outcomes for lead-poisoned children in Providence, is one.
Much of the evidence based on causality – the science of looking at observed relationships between cause and effect – can often be flawed by a misuse of cross-sectional research design as well as the misunderstanding of the different types of risk.
The use of data as evidence
I wonder: what kind of “evidence” is being developed to look at efforts now underway to determine future health care delivery in Rhode Island?
Now, don’t get me wrong. I think what the forces behind the Rhode Island Foundation effort to develop plans for health, education and racial equity are wonderful.
I am just wondering a bit how their findings and recommendations might change and evolve if their deliberations had occurred after the current pandemic.
My questions are: What have we learned about ourselves, and the strengths, weaknesses and opportunities for our state’s health system – for both preventive, acute and long-term medical care services?
Would the priorities for investment in our community health and well-being be different today, with what we have seen from the epidemiologic examination of infections, hospitalizations and deaths from COVID-19?
Institutions with the power and the money often dominate a planning process, keeping it from being balanced and community-driven, in my experience.
Unless people come together and establish a common understanding of what health is and where it comes from, recommendations for future investment will be skewed toward the institutional interests of the most powerful and best financed, in my experience.
The vision for what we want in the future needs to be informed by real experiences of all members of the community, not just those now in paid government roles, those running large hospitals, and administrators of schools of Medicine.
As I write this, what keeps popping into my head are the memories of what happened to early efforts around “regional planning” to support healthy people, when the process was disrupted by those who told us told us that the government was the problem, not the solution.
“Regional planning” became a victim of those on the right who sought to eliminate comprehensive health planning that restricted those more interested in preserving their institutions or commercial gain.
My recommendations
First, I believe there needs to be a bright light, making transparent how the money from Brown University, Lifespan and Care New England – and other corporate stakeholders such as CVS and commercial insurers – will flow into the “planning and design” of the process for consolidation of our major health services institutions.
How will these large and politically connected entities invest in ways that serve the interest of the under-represented? Is there a way to follow the money?
Second, will the Rhode Island Foundation commission a “follow-up” report to its stakeholders, analyzing the lessons learned from the coronavirus pandemic, as a way to influence future deliberations around what will make Rhode Island the healthiest state in the nation?
Third, what research and studies are being commissioned now to look at the longitudinal outcomes of health during the coronavirus pandemic in Rhode Island, tied to neighborhoods and minorities?
To read the article in its entirety: http://newsletter.convergenceri.com/stories/trouble-ahead-trouble-behind,6125
Dr. Peter Simon is a frequent contributor to ConvergenceRI.

Richard Asinof is the founder and editor of ConvergenceRI, an online subscription newsletter offering news and analysis at the convergence of health, science, technology and innovation in Rhode Island.
