Search Posts
Recent Posts
- Rhode Island Weather for June 9, 2025 – Jack Donnelly June 9, 2025
- Our Networking Pick of the Week: Uncle Jay’s Traveling Breakfast Network June 9, 2025
- When favorable treatment looks like discrimination – Mary T. O’Sullivan June 9, 2025
- To Do in RI: Literary Walking Tour, Discussion with writers in residence at Linden Place June 9, 2025
- New report recognizes music’s therapeutic and financial value in Alzheimer’s care – Herb Weiss June 9, 2025
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.

TOP STORY: The impact of the closing of Memorial Hospital in Pawtucket
(The top read story of the week was the report on the impact of the closure of Pawtucket’s Memorial Hospital on the community, the rest of the state, and the healthcare and hospital system. Now that we have the study – what is the next step – squarely in the responsibility of the RI Department of Health.)
The Rhode Island Department of Health Community Health and Health Systems Impact Assessment Related to the Closure of Memorial Hospital of Rhode Island Report, February 2020 was released yesterday.
The report looked at the impact of the closure of Memorial Hospital in Pawtucket on area hospitals, on the immediate service community of Pawtucket, Central Falls, and an area of Cumberland immediately adjacent to Central Falls, and on the state’s hospitals.
The overall conclusion is that the closure of Memorial will have long-term impacts on the community and other area providers in the absence of strategies to mitigate those impacts.
The population, compared to the rest of the state are:
o More likely to be of a racial minority,
o More likely to identify as Hispanic/Latino, Portuguese, or Cape Verdean, and more likely to speak Spanish.
o More likely to be uninsured or have public health coverage.
o More likely to live in poverty, be unemployed, and have less than a high school
education.
o More likely to live in a household without a vehicle.
Mental Health Emergency Visits
Mental health emergency department visits to Memorial had increased steadily from 2013 to 2017, with the third highest percentage in the state in 2017, the year the hospital closed. The Miriam Hospital had the largest percentage in mental health related emergency department visits during this same period.
Impact on The Miriam Hospital

With the increase in visits from the Memorial service area, longer wait times are experienced. There is a general increase in the number of hospitalizations from service area residents in part due to admissions from higher ED volume. Focus group reports have noted patients leaving prior to treatment in some cases, due to the wait times.
Conclusions:
1. The closure of Memorial removed a “nucleus” of health care services for communities with high healthcare need. Although inpatient utilization had declined over the years, residents
continued to use emergency services, hospital outpatient services, and ancillary services
located on the Memorial campus.
2. The closure of Memorial’s emergency department reduced access to emergent/urgent care services for service area residents.
3. The closure of Memorial’s emergency department reduced access to primary care services for the service area population and demonstrated the need for enhanced primary care within the service area.
4. The closure of Memorial’s Emergency Department reduced access to emergency mental health and substance use services for service area population.
5. The closure of Memorial eliminated a teaching facility for Family Medicine Residents and Internal Medicine Residents, leading to reduced number of resident slots allocated by CMS to Care New England. The immediate impact reduced primary care capacity within the Family Care Center/Internal Medicine Clinic, with a potential for a greater long-term impact, should the residency program be further cutback or eliminated.
6. Due to the impact of the closure, the mitigating strategies must take into consideration the
findings from the health needs assessment.
7. The health care needs of the community also affected the hospitals that now serve this
population, or a greater percentage of this population. The service area population is more
likely to be living in poverty, and more likely to have public insurance or be uninsured,
resulting in shifts in payer mix for area providers now serving this population.
Memorial was a significant provider of emergency care for the service area residents. From 2011-2107, they provided 6.22% of the emergency visits statewide, but 37.06% of the emergency visits for their service area residents, and residents of Pawtucket and Central Falls were particularly dependent upon Memorial for inpatient services.
Recommendations include:
Maintain and promote a health care campus at the former Memorial Hospital campus or other community-supported location that maintains access to affordable primary care and specialty services for the service area population.
Continue to offer transportation for patients residing within the service area that require care at Kent Hospital and need transportation support. Provide transportation for the caregiver to accompany patient, if indicated.
Can’t Get There from Here – Transportation/Vehicle access/Walkability
The recommendation for transportation to continue to be provided to Kent Hospital, the closest Care New England Hospital does not take into consideration the other findings in the report that speak to transportation. An obvious roadblock to patient centric care is that one hospital system will not provide transportation to another hospital system – the closest hospitals being The Miriam Hospital, Rhode Island Hospital or Roger Williams Hospital. By transporting to Kent, you now have a stranded population with “no way home”, and inaccessible to a large majority of family members and caregivers.
Households in the Pawtucket and Central Falls area have a greater percentage of people with no vehicle than the remainder of Rhode Island.
Memorial was described as a very accessible (i.e., walkable, easy parking) and familiar hospital. Walking to the hospital, taking a short car ride or using a bus, as the hospital was on a major bus line) was noted, in contrast, to travel getting to other hospitals. The Miriam Hospital, the closest to the service area, was described as more difficult to access. Several key informants, including those within the medical community, talked of patients putting off care due to travel difficulties. Some community members described their own situations where they delayed their care due to travel requirements or inconvenience. The ability for residents to walk to MHRI was mentioned often in the report.
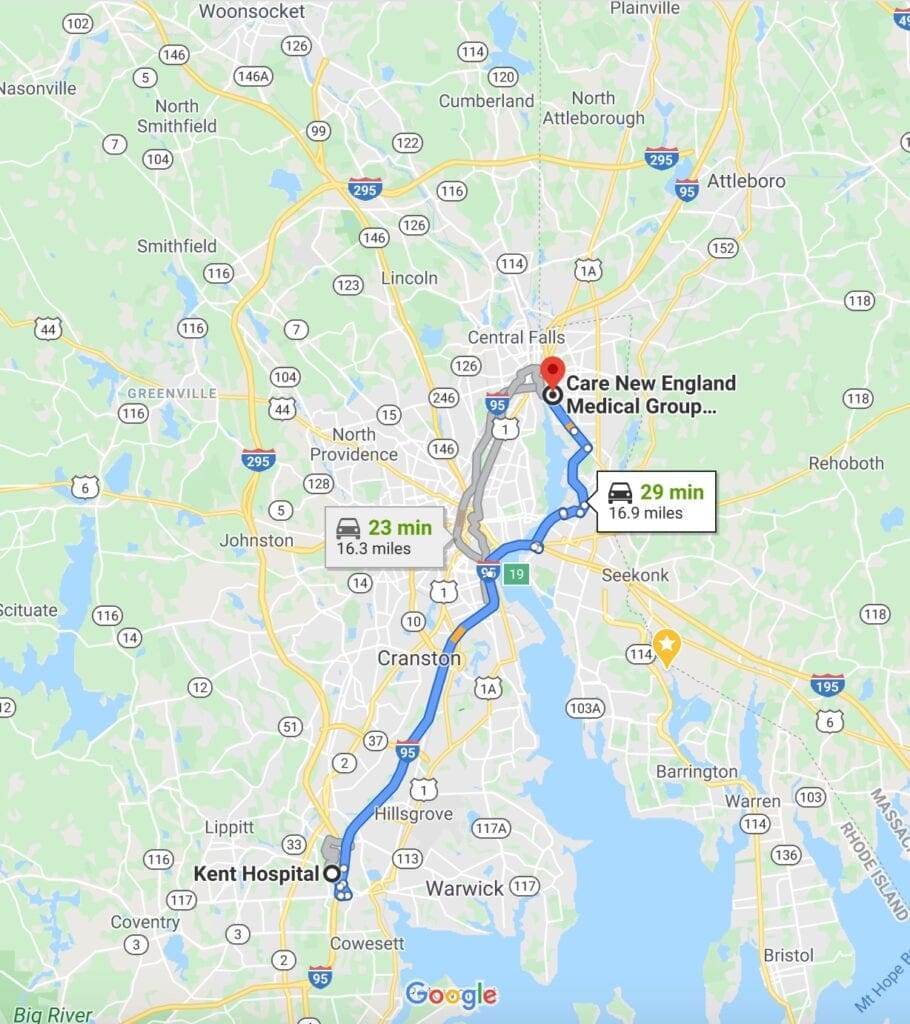
Staying within the Care New England system, Kent Hospital is the closest acute care hospital, approximately 25 minutes by car with no easily accessible public transportation. The distance and transportation barriers make it difficult for family members to visit patients during their hospital stay. Memorial patients served at Kent, who would in the past have walked to the hospital, now take Uber or Rhode Island’s non-emergency medical transport (NEMT) to access health care services or have disengaged from care and would rather not go elsewhere due to travel, inconveniences or unfamiliarity. Reliance on public transportation to utilize hospitals and other health care providers could negatively affect access to care for this population.
To view the full report with data charts, go to:
https://drive.google.com/file/d/1mmOBPGaPg7WOneCmQg65XrSppcipEWXd/view
