Search Posts
Recent Posts
- RI Veterans: Did you know? 12.06.25 (Memorial Day, Vets Cemetery, Events, Resources) – John A. Cianci June 12, 2025
- We Cook! Mill’s Tavern’s Mediterranean Seared Salmon, Olive Tapenade, Artichoke Hearts, Roasted Red Pepper Tahini June 12, 2025
- Why more Rhode Islanders are choosing Heat Pumps over traditional AC this summer June 12, 2025
- CNAs to be trained at URI in administering medication in state facilities June 12, 2025
- Rhode Island Weather for June 12, 2025 – Jack Donnelly June 12, 2025
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.

The Dictatorship of the False Equivalents – a short story – Michael Fine
By Michael Fine
© Michael Fine 2022
This is a work of fiction. Names, characters, businesses, places, events, locales, and incidents are either the products of the author’s imagination or used in a fictitious manner. Any resemblance to actual persons, living or dead, or actual events is purely coincidental.
What’s amazing about human beings is that we have the capacity to think and don’t use it. We have the capacity to feel but don’t risk relationships for fear of being hurt in them. We choose easy distraction over more satisfying work and the embrace of the miracles made every moment in being. Man is born free but everywhere is in chains. We settle. We don’t select. We choose self over soul. The universe beckons and we turn on TV. We have eyes but we see not. Ears but we hear not. We can taste and smell, but we eat at McDonald’s. And burn through our miserable little lives as if they had no value and no meaning, failing to love, failing to hope and to dream because we are afraid, making those lives miserable and little because of our fears, when life is big, mysterious, and replete with miraculous opportunity.
Why is that?
She is not safe in her home. I am sorry to have to say this, but she is not safe and there is no way we can provide services safely
That woman, Elinor Mendez is a forty-seven-year-old Hispanic female who lives on the third floor of a triple decker in Valley Falls with her husband Manny, who is a plumber. She has limb-girdle muscular dystrophy and is progressively losing function. No. It’s worse than that. She has limb-girdle muscular dystrophy, a progressive paralysis, which she inherited from her mother who died at 52 in Zambarano Hospital after spending ten years there on a ventilator. Elinor can’t take care of herself now. She is on a ventilator, at home, in a third-floor walk-up and is alone most of the day.
Limb-girdle muscular dystrophy is an inherited progressive paralysis. There are many different subtypes with different genetics: some are autosomal recessive, which means the disease only appears when a person inherits the gene from both parents. Some are autosomal dominant, which means the disease is inherited if a person gets just one gene, from only one parent. Some types of muscular dystrophy are sex-linked, which means only the male (more common), or the female children of an affected parent get the condition.
Elinor’s muscular dystrophy is autosomal dominant, not sex-linked. Her children had a fifty percent chance of getting it. She was born in 1963, before genetic testing. And she had her kids young, before genetic testing as well, although her family, which was from the Dominican Republic on her mother’s side and from Colombia on her father’s side, wasn’t that tied to health care and our science, so it isn’t clear if Elinor would have had genetic testing if it had been available. But Elinor was born here and went to high school and community college here. She worked for years at the hardware store on Broad Street in Valley Falls, which was where she met Manny. So, she is as American as apple pie.
He is a hot ticket, that Manny. He likes to dress flashy, and he loves those old cars, those old Lincoln Continentals. He drives one that is all decked out with fancy rear lights and chrome hubcaps when he’s not driving his step van, the one he uses for work. He is a hardworking man. Always has a few jobs going at once. He keeps the triple-deckers in Valley Falls and Central Falls going all by himself. He’s always rebuilding broken-down boilers or fixing the pipes that burst in the winter. He carries the new hot water tanks into the basements of all those houses on his back. Carries the new toilets up to the third floor when one of those of those old triple-deckers is getting renovated, if they ever get renovated, by himself, on his own back.
But that means he can’t sit with Elinor much. He comes by two or three times a day to check on her. You have to give him that.
So, Elinor is alone most of the day. She has two green singing finches in a cage by the window. And an orange calico cat with different colored eyes she loves. But she’s alone, and all by herself, for hours at a time, from the time our CNA leaves until Manny comes home, usually long after dark.
Elinor has been a client, on and off, for almost twenty years. First, when she was in her early thirties, Elinor lost some strength in her legs. It was barely noticeable at first. She had trouble running. Little things, like climbing stairs or getting up onto a bar stool, became difficult. We sent in a physical therapist once a week and a nurse to do an assessment, because, truth be told, she wasn’t homebound then and didn’t really qualify for services, but we took her as a client anyway because her doctor ordered the service, and with her diagnosis, no bureaucrat was going to give us a hard time, not then.
Sometimes Manny would get mad and fire us. Sometimes we had an aide who didn’t show. Sometimes we were short of aides. Young people don’t want to do this work anymore. They don’t want to work, do real work, lifting and cleaning. They all want to work from home and do IT. So, we rely on immigrants, and they are hard to get from time to time, when we are building a wall and so forth. So sometimes we’d have to cut back on Elinor’s hours. Sometimes an aide would lose something in the house, and Manny thought the aide was stealing. Sometimes the aide was stealing. One nurse took some of Elinor’s medicine. We fired her but Manny didn’t understand. So, he’d fire us and find someone else, some other agency. But then they’d find out that all of us, all the agencies, are pretty much the same. And then they’d hire us back.
Over time, Elinor lost the strength in the muscles of her thorax, in her belly and chest, the muscles that help you sit and stand, the muscles that help you lean forward and straighten up again, so it became difficult for her to get into and out of a car. She had trouble cleaning the house and needed assistance with that. We sent in a home health aide four hours a week. Manny helped as much as he could, but he works ten or twelve hours a day, sometimes more. The home health aide went to eight hours a week. Physical therapy became twice a week. Then three times a week. The home health nurse went once a month. Then once a week. We added occupational therapy and social work. Then we made the home health aide four hours a day, which is the maximum Medicare and Blue Cross allow. Anyone who needs more time than that, the regulations say, needs nursing home level of care. You can’t leave them at home. It isn’t safe.
But the disease got worse anyway. First Elinor needed a special van with hand controls so she could drive. Then she could only walk with braces for her legs and crutches. Then she needed a wheelchair. Then she stopped driving. Then her diaphragm, the big muscle that divides the chest from the belly, started to fail, and she couldn’t breathe, so she had to go on CPAP and then BiPap, special machines that blow air into the lungs under pressure, to expand them, because her body couldn’t expand and contract her lungs by itself. She got pneumonia and had to go into the hospital for weeks at a time because her lungs couldn’t expel mucus and because she couldn’t swallow correctly anymore – the muscles which control swallowing and direct food into the stomach instead of the lungs had become affected. Then she went on a ventilator, and finally had a tracheostomy, a surgically created opening for a breathing tube, placed at the bottom of her neck, and she was bed bound from then on.
And all this time, whenever she wasn’t in the hospital, she was home.
Elinor had three children, two boys and a girl. They helped as much as they could. But by the time Elinor needed the ventilator, they were all in their thirties and had lives of their own. None of them was affected, thank God. They hovered around and did what they could. The first genetic tests were developed when they were in their teens, and everyone sweated when they had those tests until the tests came back. They were lucky in that way, because they beat the odds. But not so lucky, because their mother had a debilitating disease that would kill her in her fifties, in a way that tore their hearts out.
Elinor loved her little apartment, sitting up there on the third floor on that hill on Clark Street. That apartment, sitting on the top of a hill, has amazing light. You can see over to the Blackstone River. Over to the millponds that sit between Valley Falls and South Attleboro – all the mills that are still standing and the fields of rubble where the mills used to be, where they burned down or got consumed by a friction fire, where the insurance rubbed up against the mortgage and the owner wanted to take the insurance money and sell the land, to take that money and run. You can see over to where Ann and Hope used to be, the old Lonsdale Mill. To the hills of Cumberland to the north and Scituate and Foster and Connecticut to the west. When the sun sets over those hills there is a certain beauty as the red and golden light of the setting sun reflects off the river and those millponds, as the sun goes down and then the clouds on a spring or fall day ignite, purple and orange and red. You can hear the trucks on Route 95, the rumble, sputter, cough and spit as they accelerate, and the whine of the overpowered crotch-rocket motorcycles racing with them, but you learn to ignore all that.
Elinor just heard her finches singing. She kept a radio on in the background that played Spanish music, and she spent her days propped up in bed, watching TV and talking on the phone. Manny worked with the occupational therapy people, and they rigged up a device that let Elinor work the TV and the phone with her mouth. He says she’s fine over there in that house all by herself, that she can call for help using that device, but we don’t think so. It isn’t enough. It isn’t safe to let a woman on a ventilator stay alone in a house by herself six, eight or ten hours a day.
We are responsible for the health and safety of our patients. We supply home health services to hundreds of patients, and help many people stay in their own homes. But we cannot subject our staff or our organization to liability. Medicare and the State Department of Health evaluate us continuously. We can be sanctioned for permitting unsafe living conditions for our patients. They might fine us if we let her stay at home. We could even lose our license.
It wasn’t safe for Elinor to be by herself in that house alone. What if she fell out of bed? What if the ventilator became disconnected?
I won’t live forever. None of us will. I know that Elinor thought, when Manny read her the letter from the home health agency. That letter came with two others, a letter from Medicare and a letter from the State Department of Health. They were all written in gobbledygook, some strange language that looked like English and sounded like English but had no meaning whatsoever, at least not when you read it the first time. Manny read the letter from the home health agency three or four times out loud before Elinor began to understand what it meant. Manny read slowly, with long pauses, as he tried to figure out where what words went together, to sound out some of the unfamiliar words and to make sense in his reading of how the parts of the sentences fit together.
The letters from Medicare and the State Department of Health made even less sense, no sense whatsoever, really, regardless of how many times Manny read them. They were all about Denial of Service, whatever that means, and about the discontinuation or reduction of a previously authorized course of treatment, and they talked about internal and external review and the right to appeal, and about something they called a State Fair Hearing, all of which seemed meaningless.
Elinor gestured with her mouth and eyebrows. Manny used a little syringe next to the bed to suck air out of a little valve next to Elinor’s neck and then he put a little plastic cap on Elinor’s trach tube. It was a specially designed tube for people like Elinor who lived on a ventilator. When you capped the tube like that Elinor could speak for a few minutes until she tired out. Then Manny would have to take the speaking cap off the trach tube and reinflate the balloon and let the vent breathe for her again.
“They are stopping my aide,” Elinor said.
“They can’t do that!” Manny said. “How can we manage without the aides?”
“They said they were going to do that,” Elinor said. “The social worker came. Now it’s real. There is a date. They don’t think it’s safe for me to be here. They don’t think it’s safe for me to be home alone in the afternoon.”
“So why don’t they send an aide in the afternoon, then? And in the evening to make you dinner?”
“Rules,” Elinor said. Her face became pasty as her breath started to get short. “Only. Four. Hours. A day.”
“So, what are we supposed to do?” Manny said.
Elinor shrugged. “Nursing home.”
“You don’t want that. I don’t want that,” Manny said.
Elinor shrugged again, parsing her breath, saving it for when she absolutely had to speak. Her face showed her sadness, her resignation, and her courage in the face of everything, as these different emotions washed over her.
“What. are. we. going. to do?” Elinor said, and shrugged again, now certain of the inevitability of this hated choice.
Manny knew, and Elinor knew, what the nursing home represented. Her mother had lived ten years in Zambarano Hospital, the hospital of last resort, way out in the woods, in Burrillville, twenty miles from nowhere. She lived in a tiny room with a roommate who was also on a ventilator. The nurses and CNAs came in and out of her room according to their schedule, not hers. They fed her and turned her and checked her vital signs four times a day. They washed her and dressed her and pulled her up in bed. The ventilator sat by her bedside, whooshing and hissing as it pushed air into her lungs, and as that air escaped. Elinor’s mother’s mind was good but her spirit, her soul, was trapped. Her husband, Elinor’s father, came and went. He was a good man. A patient man. But he had a wife and three children who were all dying slowly of the same dread disease. He did the best he could, but Elinor’s mother’s life was not real life. Breathing. Existing, perhaps. But not living.
“What do you want?” Manny said, although he knew the answer already. What Elinor wanted was something Manny couldn’t give her. She wanted her life back, her regular life.
Elinor shrugged. She didn’t want to be a burden on Manny. She didn’t want to be a burden on anyone. She wanted her life back, which she couldn’t have. She was ready to die, but she didn’t want to die. Despite it all, she loved living. She loved her house. She loved her children. She loved the green singing finches. And she loved Manny, although not as much as Manny loved her and not in the same way. Now it looked like she wasn’t going to be able to have any of it.
“They have their rules,” Manny said. “I hate those rules. They are protecting themselves, not caring for you. Not caring for us. Their rules say you have to be safe. What they call safe. I say you have to be free, that you should live as you choose. You might die. Everyone might die. It’s not the same. Rules on one side. Living or dying on the other. Living and dying don’t matter. All they care about is that they might get blamed. All I care about is that you should have what you want, to be what you want, to live how you want. To be here with me.”
“You. Think?” Elinor said.
“We will be fine without them,” Manny said. “We will live our lives our way. Let them go to hell.”
“Not. Hell,” Elinor said. And she smiled, as if to say, forgive them Manny, they’re just doing their jobs.
“You want someone with you all day like they say?” Manny said. “I can hire someone if I have to.”
It will bankrupt Manny, Elinor thought. I’m ok. If I died before I wake.… she thought and smiled to herself. He loves me, that man. He doesn’t want to give me up. She was tired, so tired. But I love life, and I can keep on living until I can’t. Poor Manny. He works so hard…
“I. Don’t,” Elinor said.
Then Elinor gestured. Her face was white and pasty. Wet, because she had started to sweat. Manny took the trach cap off, reinflated the balloon with the syringe that lay next to Elinor. The ventilator whooshed and hissed. Elinor pinked up. Manny closed the curtains, so the red and golden light of the setting sun didn’t fall directly on Elinor’s face. The setting sun came through another window and lit up the room anyway.
And then Elinor fell asleep.
The complaint to the Division of Facilities Regulation was routine. A patient with muscular dystrophy who was bed bound and ventilator dependent had been abandoned by the home health agency that provided her care for eight years. It was an anonymous complaint, as most complaints are, so it likely came from a disgruntled employee of the home health agency itself, or perhaps from a family member who felt guilty about what they weren’t doing to help. There’s lots of guilt out there. We pay CNAs, Certified Nurses’ Aides, ten or twelve dollars an hour. They are entry level jobs, that require only a GED and a hundred hours of training.
CNAs can take vital signs, but no one believes they are accurate. They can’t pass meds or do dressing changes. They can’t monitor a patient’s physical condition, which means they can’t listen to lungs, or the heart and they certainly can’t check the legs for swelling. They can’t start IVs or change IV bags. They certainly can’t ever touch a ventilator. Even if the ventilator hoses should become detached from the trach tube itself, they aren’t really supposed to re-attach it. Not to re-attach it would lead to the patient’s death. Instead, they are supposed to call someone. But if they did that, if they took the time to call someone, the patient would surely be dead by the time help arrived.
What actually happens in the field, in patients’ homes, is entirely different, of course. We pretend we don’t know that CNAs often do more for patients than they should. But we can’t ever acknowledge or condone what happens out of our purview. When a tree falls in a forest….
CNAs can’t do anything that looks remotely like nursing – the nursing unions see to that. They go to the legislature and complain any time someone wants to make one tiny change to the CNA scope of practice. All CNAs can do is make beds, do the laundry, and bathe someone who is home bound.
Most CNAs don’t belong to a union. So, they complain every time someone asks them to do something they don’t want to do.
We followed the correct procedure. We determined that the patient required a higher level of care than we could provide. We notified the patient and their family, the State Department of Health, and CMS that the patient’s needs exceeded our licensed capacity. We provided thirty-day notice, and the opportunity to appeal. So, I was and am confident that our decision will be supported by all regulatory authorities, and so we will cease providing services on a date certain.
That lady can’t do nothing for herself. And they think I don’t know nothing.
I walk up two flights of stairs to her house every day.
Some people, they are never satisfied. Bring me this. Bring me that. I’m too hot. I’m too cold. Fix the pillow. No, you got it wrong. Fix the pillow again. The bottle goes in the recycling, not in the trash. Don’t you know nothing? And I know you people. I’m watching you every second. I know you people steal.
Not her. She happy to see me. She happy when I turn her. Happy when I wash her. Happy when I pull her up in bed.
If I were that lady maybe I be mad her husband doesn’t stay with her all day. But she don’t do mad.
I’d be mad, if I was her, stuck in the bed like that with the machine next to her bed, whooshing like the brakes on a bus, in and out, in and out. Not her.
Now they don’t want me to come back no more. What’s she gonna do, that woman?
They got their rules. This lady’s gonna die anyway but she will die in a mess, by herself, if they don’t send someone every day to clean her up.
You can’t talk good to evil.
They say you got to follow the rules. But their rules don’t make no sense.
I went myself on the last day. We had followed the correct procedure. You can’t put an entire agency at risk for one person. Elinor was not at a homebound level of care. No ventilator patient is. She wasn’t even at an assisted living level of care. The rules and guidelines were clear. Elinor was nursing home level of care. We had done everything we could to convince her to go into a nursing home. Social work. Psychiatric assessment. Motivational interviewing. Shared decision making, the whole nine yards.
It was the last day of May. Memorial Day had come and gone. The sun was strong and hot, even first thing in the morning. The beaches had opened. School wasn’t out yet but the kids on the street could taste the coming summer. They wore shorts and t-shirts and pushed and prodded one another as they waited for the school bus in the morning, or as they walked to school.
Elsie, the aide we had with Elinor, was a Honduran woman in her thirties, a hard worker but very quiet. She was short and strong; with deep dark brown eyes and long dark hair she wore up and kept in a hairnet while she worked. The aides all knew not to get too attached to Elinor. That she wouldn’t live forever. They know that about many of our patients, but it is easier with the old ones, those who will die after a long life well lived. Young people are harder. The aides see themselves in those people; they see them as friends, as sisters and brothers, and their deaths are devastating when an aide gets too close.
Elsie moved from room to room, carefully following the home health assessment and plan of care that had been written by Elinor’s nurse, approved by her doctor, and was submitted and resubmitted to CMS every sixty days. She washed Elinor and changed the linens on Elinor’s bed, singing to herself as she worked. She swept the floor and checked Elinor’s pulse rate, blood pressure and oxygen saturation, and recorded it all in a file folder printed in bright colors, the file folder from our agency. The green singing finches chirped in the sunlight.
I pulled up a chair next to Elinor’s bed.
“This is Elsie’s last day,” I said.
Elinor shrugged.
“It is not safe for you here.”
Elinor shook her head, as if to say, ‘That’s not true. I don’t want to be safe. I want to be here, in my own house, in this place I love. It doesn’t matter what you say.’
“I understand why you’d want to stay here.”
Elinor shook her head again and raised her eyebrows, as if to say, ‘no, you don’t understand anything. If you understood, you’d give me my aides.’
“I have no choice. You have to understand how difficult this is for me.”
Elinor shook her head. Nothing I said was going to matter. I don’t know if she believed me or not. Her heart rate, which I saw on a little screen on the vent, began to rise. She twisted her head for a moment, and she looked right at me. Right through me. I couldn’t imagine what she was thinking or feeling. The very white skin on her forehead got wet with sweat and glistened in the daylight from the window next to her bed.
The ventilator was set on rate control: so many breaths per minute, with each breath a certain volume, delivered at a certain pressure. The person on the ventilator doesn’t control any of that. The machine does. The person on the ventilator lies still and all the work of breathing is done for them by the machine.
A person on a ventilator can fight the vent – they can use their own muscles, if they have control of any muscles, to resist the pressure, or breathe faster than the machine. A part of me expected Elinor to do just that – get upset or agitated, twist in the bed with whatever muscle power she still had left, and cough against the machine. You can blow the tubing off the trach tube if you cough hard enough. You can cough yourself off the ventilator that way.
I found a facecloth and wiped the sweat from Elinor’s brow.
Then Elinor closed her eyes. Elinor’s heart rate dropped. She stopped moving her head.
And then a great peace came over the room.
Elinor wasn’t dying. She was stronger than that. She had just chosen life over us.
I would like to tell you that we changed the plan, and that Elsie stayed with Elinor until the end. Or that we broke protocol, and that Elsie and I kept coming at night and on weekends, on our own time to help.
But none of that is true. We stopped services. And we carry on as we always did. We provide services and are paid for those services, according to our contract and Medicare’s rules. Forms and rules.
Elinor lived another two years. Manny and their kids did everything by themselves. They were fine without us. I’m sure they struggled from time to time.
But Elinor and Manny lived the life they chose, a life free of rules and restrictions.
Human freedom has little to do with those rules and restrictions. Our freedom is the freedom that exists in each soul, where we choose between the rules that men make and our tiny moment of love, hope, and solidarity. Nothing could be more different.
Humans are born free. Nothing else matters.
All of Michael Fine’s stories and books are available on MichaelFineMD.com or by clicking here. Join us!
___
Read other short stories by Michael for RINewsToday, here: https://rinewstoday.com/dr-michael-fine/
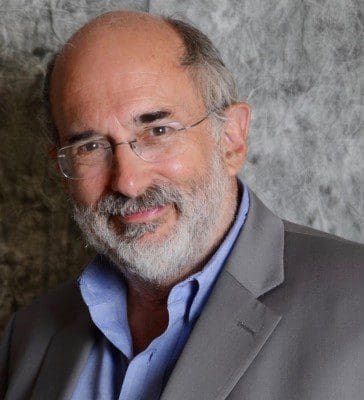
Michael Fine, MD has served as Health Policy Advisor in Central Falls, RI and Senior Population Health and Clinical Services Officer at Blackstone Valley Health Care, Inc. He is facilitating a partnership between the City and Blackstone to create the Central Falls Neighborhood Health Station, the US first attempt to build a population based primary care and public health collaboration that serves the entire population of a place.
He has also recently served as Health Liaison to the City of Pawtucket. Dr. Fine served in the Cabinet of Governor Lincoln Chafee as Director of the Rhode Island Department of Health from February of 2011 until March of 2015, overseeing a broad range of public health programs and services, overseeing 450 public health professionals and managing a budget of $110 million a year.
Dr. Fine’s career as both a family physician and manager in the field of healthcare has been devoted to healthcare reform and the care of under-served populations. Before his confirmation as Director of Health, Dr. Fine was the Medical Program Director at the Rhode Island Department of Corrections, overseeing a healthcare unit servicing nearly 20,000 people a year, with a staff of over 85 physicians, psychiatrists, mental health workers, nurses, and other health professionals.
He was a founder and Managing Director of HealthAccessRI, the nation’s first statewide organization making prepaid, reduced fee-for-service primary care available to people without employer-provided health insurance. Dr. Fine practiced for 16 years in urban Pawtucket, Rhode Island and rural Scituate, Rhode Island. He is the former Physician Operating Officer of Hillside Avenue Family and Community Medicine, the largest family practice in Rhode Island, and the former Physician-in-Chief of the Rhode Island and Miriam Hospitals’ Departments of Family and Community Medicine. He was co-chair of the Allied Advocacy Group for Integrated Primary Care.
He convened and facilitated the Primary Care Leadership Council, a statewide organization that represented 75 percent of Rhode Island’s primary care physicians and practices. He currently serves on the Boards of Crossroads Rhode Island, the state’s largest service organization for the homeless, the Lown Institute, the George Wiley Center, and RICARES. Dr. Fine founded the Scituate Health Alliance, a community-based, population-focused non-profit organization, which made Scituate the first community in the United States to provide primary medical and dental care to all town residents.
Dr. Fine is a past President of the Rhode Island Academy of Family Physicians and was an Open Society Institute/George Soros Fellow in Medicine as a Profession from 2000 to2002. He has served on a number of legislative committees for the Rhode Island General Assembly, has chaired the Primary Care Advisory Committee for the Rhode Island Department of Health, and sat on both the Urban Family Medicine Task Force of the American Academy of Family Physicians and the National Advisory Council to the National Health Services Corps.
