Search Posts
Recent Posts
- Rhode Island Weather for April 29, 2024 – John Donnelly April 29, 2024
- Advocates, providers on new Nursing Home mandates – Herb Weiss April 29, 2024
- Business Beat: Abe Cohen new VP of Business Development for RI, Marquis Health Consulting April 29, 2024
- Business Monday: Working and playing into your 90s – Mary T. O’Sullivan April 29, 2024
- Rhode Island Weather for April 28, 2024 – John Donnelly April 28, 2024
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.
Responses begin to declaration of nursing home emergency in RI
RINewsToday reached out to local groups who have been active in the minimum standards for nursing homes issue, as a follow up to the declaration of a Nursing Home Emergency in Rhode Island, made by Gov. McKee on December 29th.
John E. Gage, MBA, NHA, the President & CEO of the Rhode Island Health Care Association released this statement:
The Rhode Island Health Care Association (RIHCA) and its sixty-three (63) member nursing facilities would like to acknowledge and thank Gov. Dan McKee for issuing his recent Executive Order. This action was taken to preserve Rhode Island elders’ access to necessary short-term rehabilitative care, Alzheimer specialty care, and long-term care services in Rhode Island nursing facilities, and to ensure the sustainability of the entire healthcare continuum.

In the absence of this action, fines of more than $65 million resulting from the staffing mandate would have been issued to seventy-three (73) Rhode Island nursing facilities for the period of July 1, 2022 through September 30, 2023. For each subsequent quarter, fines would be over $20 million and over a year, fines would be nearly $100 million. Penalties of this magnitude would only serve to hasten further closures, receiverships, and bankruptcies. Residents would be discharged from their homes. Staff would be displaced from their jobs. Hospital capacity would be strained as nursing homes would not have the capacity to accept patients resulting in the boarding of long-term care patients at the wrong level of care and costing hospitals millions of dollars. Resident care would be devastated – the very care that the staffing mandate was intended to improve.
· The Nursing Home Minimum Staffing Statutes were enacted in May of 2021. The estimated cost of implementing the mandates is more than $60 million/year while it provided just $12 million/year after the third phase of labor add-ons being implemented October 1, 2023 – leaving a $48 million unfunded mandate.
· This $48 million annual shortfall is on top of the structural estimate of $50 million/year resulting from more than a decade of chronic Medicaid underfunding resulting from more than a decade of sequential inflation index cuts (2012 – 2021) and Medicaid’s failure to conduct the statutorily required rebase of the price-based reimbursement system since its inception in 2012.
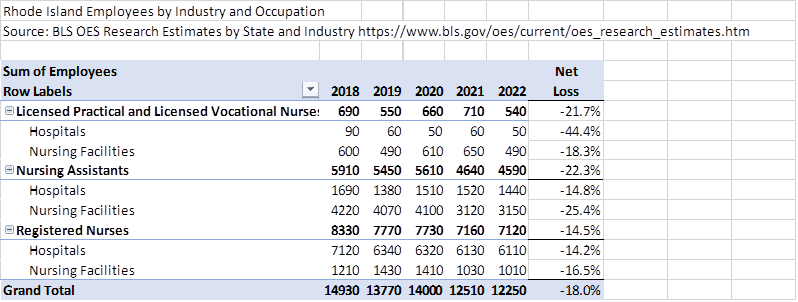
· To further complicate matters, the staffing mandate was implemented during the Covid-19 pandemic which devastated the nursing home workforce. The most recent BLS statistics indicate that Rhode Island’s nursing facility workforce is down some 18% from pre-pandemic levels. A detailed analysis of the workforce for hospitals and nursing homes is below. It demonstrates that nursing home RNs have declined by 16.5%, LPNs by 18.3% and CNAs by 25.4%. It is estimated that, nationwide, recovery of the nursing home workforce will not occur until 2027 based on the small, incremental improvements quarter over quarter.
· Given the absence of a sufficient available workforce and the lack of adequate funding, 93% of facilities statewide were unable to achieve or maintain compliance with staffing requirements throughout this period and would have been fined.
· Fines of hundreds of million dollars would siphon off already scarce, mostly Medicaid revenues from facilities, their ongoing retention and recruitment efforts, and would upend resident care. Further facility closures would be an absolute certainty.
· Since the beginning of the pandemic in early 2020, six (6) RI nursing homes have already closed – Apple Watch Hill (Westerly), Ballou Home (Woonsocket), Hallworth House (Providence), Woodpecker Hill Health Center (Greene), Elderwood at Riverside (East Providence) and Charlesgate Nursing Center (Providence) as the direct result of the financial strain resulting from insufficient Medicaid reimbursement, an unprecedented labor crisis, skyrocketing wage-pressure and the last-resort reliance on costly staffing from nursing service agencies.
· In addition, three (3) RI nursing facilities are currently in receivership because of significant operational and financial challenges. These include Pawtucket Falls Nursing Center (Pawtucket), Hebert Health Center (Smithfield) and Trinity Health Center (Woonsocket). In addition, other facilities such as Linn Health and Rehabilitation have recently gone public with their dire financial struggles.
___
James Nyberg, MPA, Executive Director of LeadingAge RI also released a statement:

Nyberg says he “appreciates the Governor taking this initiative to provide relief to nursing homes regarding the minimum staffing ratio fines. It recognizes both the draconian nature of the fines and the practical reality of the workforce shortage in health care, let alone the financial crisis that is already engulfing the industry and threatening more closures, which we are all trying to rectify. We all support adequate staffing in our nursing homes to care for our residents and look forward to working with all stakeholders on a path forward for a financially sustainable nursing home industry.”
__
Maureen Maigret, the Policy Advisor for the Senior Agenda Coalition of RI also responded to the article with this statement:

“The Senior Agenda Coalition of Rhode Island has a long history of working to support adequate staffing in our nursing homes to ensure quality care for their residents. As our state’s population grows older, it is critical that we have a sufficient supply of quality nursing homes. This is especially important because Rhode Island has such a high percent of persons aged 85 and over and persons in this age group are more likely to need the level of care provided in nursing homes.
While the Governor’s Executive Order puts the penalty provisions for failure to comply with the staffing requirements on hold, state government must seek longer-term solutions to this issue. It is necessary that a comprehensive examination of the issue of nursing home financing, including the adequacy of Medicaid reimbursement rates as well as the role and impact of private equity and corporate ownership takes place. And equally as important to accelerate efforts to address the workforce crisis impacting long term care and healthcare in general.
UPDATED:
Jesse Martin, Executive Vice President of SEIU 1199NE and member of Raise the Bar on Resident Care Coalition, issues the following statement:
“Governor McKee signed The Nursing Home Staffing and Quality Care Act into law in 2021 after a majority of COVID-related deaths were found in nursing homes and assisted living facilities. Although studies have shown that safe staffing is the primary way to ensure quality care, Rhode Island now ranks 38th in the country according to the AARP. While many of our state’s non-profit homes have exceeded safe staffing requirements, the majority of for-profit nursing homes continue to rack up massive profits while crying wolf about safe staffing fines. Instead of giving nursing home owners free rein, it is critical that all stakeholders work together to hold nursing homes accountable to providing safe, dignified care.”

Raise the Bar on Resident Care is a coalition of nursing home caregivers, clergy members, community partners, nursing home residents, and family members working to end the staffing crisis in Rhode Island nursing homes.
___
This is a developing story
Yesterday’s article, including the full context of the Executive Order:
___

The feds should redirect foreign aid from countries that violate international law and send to to boost the Medicaid programs in certain states.