Search Posts
Recent Posts
- Rhode Island Weather for June 4, 2025 – Jack Donnelly June 4, 2025
- Sour Grapes time! – Tim Jones (meet Tim at AnimeCon) June 4, 2025
- Lawsuit filed to stop Empire Wind Project by 4 environmental groups and fishermen June 4, 2025
- It is what it is: 6.4.25 – Jen Brien June 4, 2025
- New ALS treatment by PathMaker Neurosystems. Co. funded by RI Life Sciences Hub to come to RI. June 3, 2025
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.
Regulatory approval can make a belated Christmas miracle happen – Herb Weiss
Regulatory Agencies Approval Can Make Facility’s Belated Christmas Miracle Happen
By Herb Weiss, contributing writer on aging issues
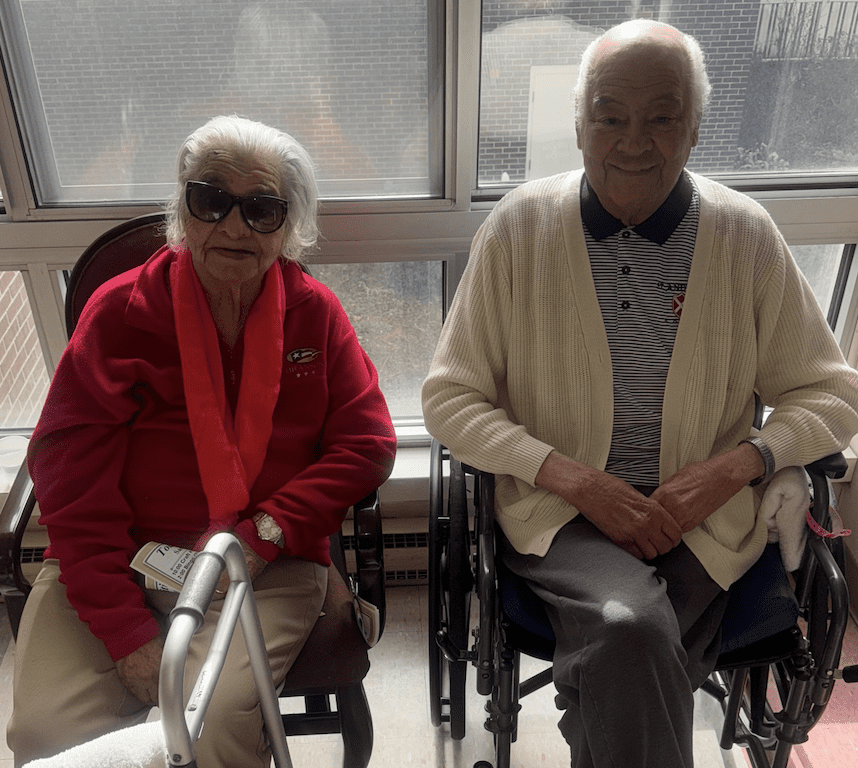
Photos – Linn Health
A belated Christmas miracle may truly happen, if state and federal agencies allow the Linn Health & Rehabilitation to convert one of its floors into affordable assisted living specializing in memory and dementia care. If this happens, says the facility’s management and its Board of Trustees it will keep the East Providence-based nonprofit facility from closing, preventing the displacement of residents and staff.
Faced with rampant inflation, rising food and utility costs, high temporary staffing agency fees, and very low state Medicaid reimbursement rates that haven’t kept pace with increasing costs in over a decade, Linn Health, established over 52 years ago, publicized its financial troubles over four months ago.
The Best of the Best
When the news broke about Linn Health & Rehabilitation’s financial crisis over four months ago, the facility had just been named a 2024 ‘Best Nursing Home’ and ‘High-Performing’ short-term rehabilitation home in the nation by U.S. News & World Report, states Jamie L. Sanford, LNHA, LCSW, administrator of Linn Health & Rehabilitation.
“Here we are, one of the elite nursing homes in the United States, and we are finding it difficult to stay afloat like six other homes in our local market who have gone out of business, and three others who have declared bankruptcy, and one other who recently had to downsize by 50 beds,” says Sanford.
“It’s sad that Rhode Island families who deserve an affordable 5-star nursing home like ours don’t have the option because of inadequate Medicaid reimbursement. The struggle is real,” says Sanford.
Together with Aldersbridge Communities and its volunteer Board of Trustees, Linn leaders launched a savvy PR move, calling it a “Hail Mary” effort, to find its Christmas miracle donors and funding to prevent it from closing or forcing the displacement of 71 residents and the laying off of 150 staff members. A clever twist on the message resulted in a story on Rhode Island television stations, talk radio, and pick up by other media outlets.
“Our tireless pleas for funds to keep us afloat until a slight Medicaid reimbursement rate increase is expected to take place later this year were heard, but didn’t result in us receiving any emergency gap funding. We did receive charitable contributions from generous donors in earnest, but the amount was nowhere near enough to cover our losses of $100,000 per month,” states Richard Gamache, MS, FACHCA, chief executive officer of Aldersbridge Communities. With revenues dwindling, Linn leadership came up with a solution: convert one floor of the nursing home into affordable assisted living, specializing in memory and dementia care”, he notes.
Submitting the Application
According to Gamache, its application for recertification was submitted last month and he expects the license to be approved by the RI Department of Health soon. “Obtaining our certification so that we can bill the Centers for Medicare & Medicaid Services is a bigger obstacle, because the federal government is involved,” he says. But, it could take “one or two months to get the facility’s licensing and certification approved by the RI Department of Health and Human Services (RIDHS) and CMS.
If approved and certified, Linn Health & Rehabilitation will operate “The Loft at Linn” – a new assisted living memory care unit featuring 22 private studio apartments on the second floor of the building. The third floor will remain a licensed nursing home, albeit smaller now with 33 beds.
According to Gamache, the RIDHS has recertified Linn residents currently receiving long-term care to qualify for assisted living-level memory care, enabling them to continue to live at Linn and have the same caregivers they are used to and know.
Meanwhile, grant funding from the Rhode Island Foundation, the Ruby Linn Foundation, and other sources are being used to pay for the apartment renovations; and to re-educate and train certified nursing assistants to become certified medical technicians so they can remain on staff working at the assisted living memory care program.
Shifting operations to assisted living and repurposing existing nursing home rooms will keep the facility’s doors open. “It’s not enough to solve our financial woes completely, as we expect the nursing home to continue to lose money – just not as much as we have been losing,” notes Gamache. “The irony is that we will save Rhode Island over $780,000 in a year because of the difference between what they will reimburse us for assisted living, versus a skilled level of care per Medicaid resident,” Gamache calculates.
As a whole, because we’re going from a 42-bed skilled nursing floor to a 22-bed assisted living floor, the state is going to save $2.8 million per year in Medicaid dollars,” notes Gamache.
It is not surprising that Rick Gamache, who has years of experience managing nursing facilities, might have just found a way to keep his facility open,” says Kathleen Heren, Rhode Island’s Ombudsman. If the request of recertification is approved by state and federal regulators to offer assisted living with memory care, residents won’t be displaced and workers won’t lose their jobs, says Heren.
“It was never a viable option to sell Linn Health to an out-of-state nursing facility chain,” says Heren, noting that there is a need for assisted living facilities offering memory care. “There are high functioning people affected with dementia, with no medical conditions, who do not need to be placed in a nursing facility,” she adds.
Comments from the Sideline
Like Heren, Maureen Maigret, policy advisor for the Senior Agenda Coalition and member of the RI Advisory Council on Alzheimer’s Disease Research and Treatment, holds Gamache in high regard. By converting a floor to needed assisted living with a memory care, staff will not be displaced, so residents with memory issues will not be losing staff who know them and who they are comfortable with.
According to Maigret, many assisted living residences strictly limit residents on Medicaid. A few years back, the state changed the Medicaid reimbursement for assisted living to one with three levels of reimbursement with a higher level of reimbursement to encourage more residences to accept persons with higher needs who are on Medicaid. ”We know that RI has many persons with diagnoses of Alzheimer’s and related dementias so such memory care programs are critical for those who cannot pay privately with monthly rates often over $6,000,” says Maigret.
Maigret notes that the state’s Health Department reports that 34 assisted living residences are licensed as Special Care/Alzheimer’s residences, but it is does not show which ones accept Medicaid. “And even those that do often limit the number of residents on Medicaid as they can get higher reimbursements from private paying persons,” she says.
According to Gage, in 2024, RI’s nursing homes are being paid rates by Medicaid that are based on their 2011 actual costs under the price-based reimbursement system that was implemented in 2013. Core principles of this reimbursement methodology are the statutory annual inflation adjustments and a Medicaid rate analysis every three years to determine whether rates are reasonable and adequate. “In the vast majority of years in the past decade, RI Medicaid has slashed or eliminated inflation adjustments, and they have never conducted a rate analysis/adjustment. As a direct result, RI nursing homes are losing $50-75/day on each resident receiving care under Medicaid,” he says.
Gage predicts that Linn and Scandinavian Home will not be the last to make the difficult choice to downsize or close. “Just since the start of the pandemic, six RI nursing homes have closed and three were in receivership. Now, two nonprofit homes are forced to downsize their facilities,” he noted. “RI nursing homes must be adequately reimbursed by Medicaid under a stable and sustainable reimbursement system, and there needs to be bold action to recruit and retain frontline healthcare workers at competitive rates,” he warns, calling for the state to preserve nursing facilities.
Demographics show a silver tsunami on the horizon. We need to ensure that there will be capacity for those who will need short-term or long-term care and services in the coming years,” states Gage.



As far as any potential Medicaid savings resulting from the planned conversion, Gage says that Linn would only be able to accommodate 33 nursing facility residents down from its former capacity of 87. By downsizing the nursing home by 54 beds and transitioning that floor into low-income memory care assisted living for just 22 residents, there will be a savings to the state, he says. due to the combined capacity of the facility decreasing by 32 residents, and those who remain in the memory care unit will be receiving a lower level of care and assistance than that provided in a skilled nursing home.
At press time, Gamache waits for the license from RIDOH and certification from the Centers for Medicare & Medicaid Services to be approved that enables the opening of the new assisted living memory care program.
“There is no reason while this approval shouldn’t happen,” says Gamache. “We can comply with all the regulations, we’ve identified an overwhelming community need, and we are saving the state a lot of money,” he quipped.
“After all, this is a win/win for the state, for residents, their families and staff to enable Aldersbridge Communities continue operating a full continuum of care,” states Gamache.
___

Herb Weiss, LRI -12, is a Pawtucket-based writer who has covered aging, health care and medical issues for over 43 years. To purchase his books, Taking Charge: Collected Stories on Aging Boldly and a sequel, compiling weekly published articles, go to herbweiss.com.

[…] Health sought a “Christmas miracle” (see RINewsToday story: HERE) in late 2023 to save the nursing home from having to displace […]