Search Posts
Recent Posts
- Dr. Rosemary Costigan Named President of Community College of Rhode Island June 19, 2025
- RI Veterans: Did you know? 19.06.25 (Military Funerals, Job Fair, Benefits, Events) – John A. Cianci June 19, 2025
- East Providence First in U.S. to Equip All Firefighters with PFAS-free Gear June 19, 2025
- We Cook! Mill’s Tavern Saffron Bouillabaisse with Tarhana Lobster Jus June 19, 2025
- Rhode Island Weather for June 19, 2025 – Jack Donnelly June 19, 2025
Categories
Subscribe!
Thanks for subscribing! Please check your email for further instructions.
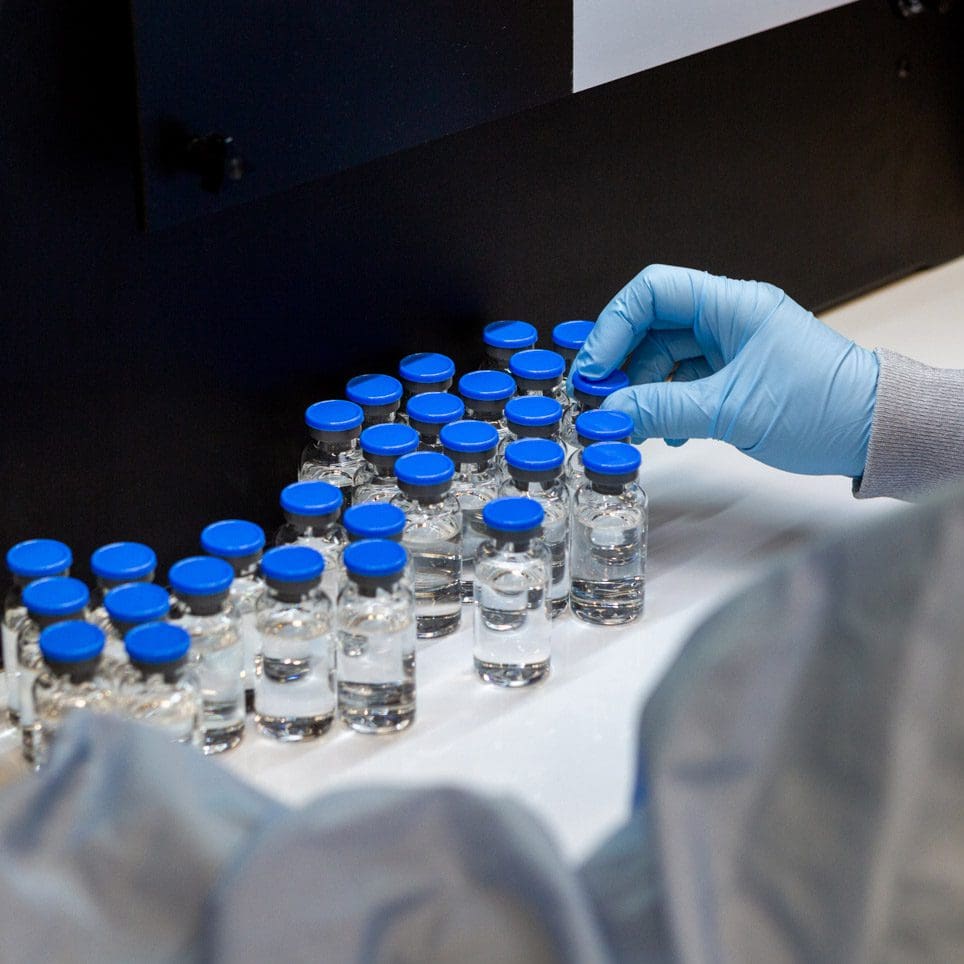
Gilead’s Remdesivir will get better and better – Dr. Anthony Fauci
Anthony Fauci, a leading member of the White House’s coronavirus task force, cautioned the trial results for the antiviral drug remdesivir were not a “knockout”. But he compared it to the early anti-HIV drug AZT, which became the basis of future treatments for that virus. “We think it’s really opening the door to the fact that we now have the capability of treating [Covid-19],” Dr Fauci said on Wednesday. “And I can guarantee you as more people, more companies, more investigators get involved it will get better and better.”
In an unannounced press event carried by only some national television networks, jumping in to see familiar faces, Dr. Fauci and Dr. Birx sitting on a yellow couch with Dr. Fauci very animatedly talking about a 10,000 person trial of remdesivir which had been stopped so they could tell the placebo group that they were not on the drug and they would be switched to it – results were that promising. The President was in the oval office along with other representatives in this event, which looked spontaneous and almost an after-thought.
Here are the details from Gilead:
Gilead Sciences, Inc. (Nasdaq: GILD) today announced topline results from the open-label, Phase 3 SIMPLE trial evaluating 5-day and 10-day dosing durations of the investigational antiviral remdesivir in hospitalized patients with severe manifestations of COVID-19 disease. The study demonstrated that patients receiving a 10-day treatment course of remdesivir achieved similar improvement in clinical status compared with those taking a 5-day treatment course (Odds Ratio: 0.75 [95% CI 0.51 – 1.12] on Day 14). No new safety signals were identified with remdesivir across either treatment group. Gilead plans to submit the full data for publication in a peer-reviewed journal in the coming weeks.
“Unlike traditional drug development, we are attempting to evaluate an investigational agent alongside an evolving global pandemic. Multiple concurrent studies are helping inform whether remdesivir is a safe and effective treatment for COVID-19 and how to best utilize the drug,” said Merdad Parsey, MD, PhD, Chief Medical Officer, Gilead Sciences. “These study results complement data from the placebo-controlled study of remdesivir conducted by the National Institute for Allergy and Infectious Diseases and help to determine the optimal duration of treatment with remdesivir. The study demonstrates the potential for some patients to be treated with a 5-day regimen, which could significantly expand the number of patients who could be treated with our current supply of remdesivir. This is particularly important in the setting of a pandemic, to help hospitals and healthcare workers treat more patients in urgent need of care.”
Remdesivir is not yet licensed or approved anywhere globally and has not yet been demonstrated to be safe or effective for the treatment of COVID-19. This study sought to determine whether a shorter, 5-day course of remdesivir would achieve similar efficacy results as the 10-day treatment regimen used in multiple ongoing studies of remdesivir. Secondary objectives included rates of adverse events and additional measures of clinical response in both treatment groups. Patients were required to have evidence of pneumonia and reduced oxygen levels that did not require mechanical ventilation at the time of study entry. Clinical improvement was defined as an improvement of two or more points from baseline on a predefined seven-point scale, ranging from hospital discharge to increasing levels of oxygen support to death. Patients achieved clinical recovery if they no longer required oxygen support and medical care or were discharged from the hospital.
In this study, the time to clinical improvement for 50 percent of patients was 10 days in the 5-day treatment group and 11 days in the 10-day treatment group. More than half of patients in both treatment groups were discharged from the hospital by Day 14 (5-day: 60.0%, n=120/200 vs.10-day: 52.3% n=103/197; p=0.14). At Day 14, 64.5 percent (n=129/200) of patients in the 5-day treatment group and 53.8 percent (n=106/197) of patients in the 10-day treatment group achieved clinical recovery.
Clinical outcomes varied by geography. Outside of Italy, the overall mortality rate at Day 14 was 7 percent (n=23/320) across both treatment groups, with 64 percent (n=205/320) of patients experiencing clinical improvement at Day 14 and 61 percent (n=196/320) of patients discharged from the hospital.
Impact of Earlier Treatment
In an exploratory analysis, patients in the study who received remdesivir within 10 days of symptom onset had improved outcomes compared with those treated after more than 10 days of symptoms. Pooling data across treatment arms, by Day 14, 62 percent of patients treated early were able to be discharged from the hospital, compared with 49 percent of patients who were treated late.
“These data are encouraging as they indicate that patients who received a shorter, 5-day course of remdesivir experienced similar clinical improvement as patients who received a 10-day treatment course,” said Aruna Subramanian, MD, Clinical Professor of Medicine, Chief, Immunocompromised Host Infectious Diseases, Stanford University School of Medicine, and one of the lead investigators of the study. “While additional data are still needed, these results help to bring a clearer understanding of how treatment with remdesivir may be optimized, if proven safe and effective.”
Remdesivir was generally well-tolerated in both the 5-day and 10-day treatment groups. The most common adverse events occurring in more than 10 percent of patients in either group were nausea (5-day: 10.0%, n=20/200 vs. 10-day: 8.6%, n=17/197) and acute respiratory failure (5-day: 6.0%, n=12/200 vs. 10-day: 10.7%, n= 21/197). Grade 3 or higher liver enzyme (ALT) elevations occurred in 7.3 percent (n=28/385) of patients, with 3.0 percent (n=12/397) of patients discontinuing remdesivir treatment due to elevated liver tests.

